Fat shaming or life saving

Introduction
In February 2004, HTV Wales made a discussion programme about obesity. They hosted a dozen people with many different perspectives on the topic to have a studio debate. I had just had a book published called “Why do you overeat? When all you want is to be slim” and I was invited. I was asked if I knew anyone who was obese and happy to be so, as they wanted that viewpoint represented. I didn’t. When I arrived for the recording, I discovered that they had found a woman to fulfil this role. They hadn’t found anyone in Wales, so they had chauffeured X from the south east of England. It turned out that X didn’t want to be obese. If there were a magic pill that she could take to be slim now and for life, she would take it in an instant. She felt that she had failed so often at dieting that she couldn’t put herself through that again and had thus made some peace with her size; but she didn’t want to be obese.
I’ve still never met anyone who wants to be obese.
Doughnut-gate
This week’s post was inspired by what has become known as “Doughnut-gate” – or “Donut-gate” for our north American friends – but it’s about much more than that. It’s about obesity. It’s about healthcare workers. It’s about what is emerging to be one of the biggest risk factors for COVID-19. It’s about what fat shaming is and what it isn’t. It’s about public health and whether the silencing of discussions about obesity could be risking lives…
On April 21st, the London Royal Free hospital tweeted the following (Ref 1):

You can see that the Royal Free tweet had 83 tweets and 1,400 likes (as of 7th May when I screen grabbed it). It also got a number of replies. The replies were polarised between ‘how nice of a company to give our treasured National Health Service (NHS) workers a ‘treat’’ and ‘how inappropriate for a junk food company to be delivering junk to a health service.’ Many replies also pointed out that this was a marketing ploy for KrispyKreme to get some of the abundant love surrounding the NHS right now.
The following morning, Dr Aseem Malhotra retweeted the Royal Free tweet calling it “absolutely disgraceful” (Ref 2).

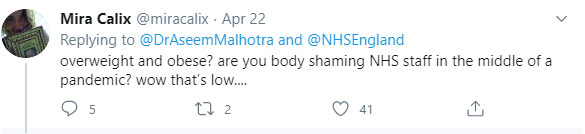
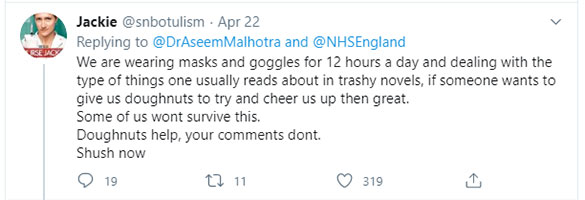
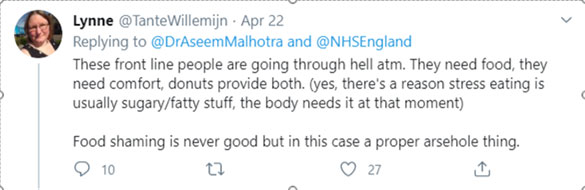
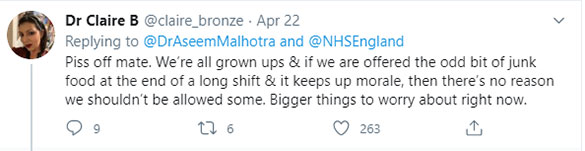
Aseem’s tweet has had 644 retweets and 2,300 likes, so you could say that he had more support for his stance – but he also has many more followers than the hospital. As with the original Royal Free tweet, the replies to Aseem were polarised. Many were supportive, but here are a selection capturing the themes of the critical replies. All but the first one are from doctors/nurses:
The two themes that I want to pick up on are:
1) The allegation that the mere mention of food or weight is “food shaming” “body shaming”;
2) The belief that KrispyKreme doughnuts will cheer people up/boost morale/alleviate stress.
Before I explore those two themes, I want to briefly address a couple of comments that said where’s the evidence that junk food is the problem? And that’s a fair point. The evidence is scant because who would fund it? Nutritional ‘science’ has been corrupted for decades (Ref 3). Organisations like Public Health England (PHE) should be funding research into the fact that obesity was 2.7% in the UK in 1972 and almost ten times that by 1999, coincidentally during the low fat/high carb/processed food era. But, instead, PHE allowed the processed food industry bodies to design the ‘eatwell’ plate for the UK (Ref 4). You couldn’t make it up.
Professor John Yudkin nailed it in his 1972 book Pure, White and Deadly: “The consumption of sugar on top of an ordinary diet increases the risk of obesity; the consumption of sugar instead of part of an adequate diet increases the risk of nutritional deficiencies.”
Back to 1) shaming and 2) cheering up…
1) The definition of fat shaming is: “the action or practice of humiliating someone judged to be fat or overweight by making mocking or critical comments about their size.”
Using the words “overweight”, “obese”, “junk food” in their normal meaning is not fat shaming or body shaming or whatever other claims people want to make. By definition – literally – it isn’t. Abuse (for that is what it is) of the words fat shaming diminishes the power that the term should carry when it needs to be used appropriately. Abuse of the term is also dangerous, as it deliberately tries to prevent discussions about vital topics – weight, food, and health. We need to be able to discuss such things – never more so than right now, as I will come on to.
2) When I have done radio interviews about childhood obesity, I have expressed one consistent wish. I wish that grownups would teach children that junk food is junk food – it is not a treat. It should not be (ab)used to cheer someone up/boost morale/alleviate stress. If a child falls over, comfort them – don’t give them junk. If a child falls out with a friend, counsel them – don’t give them junk. It’s bad enough that junk food companies make every joyful occasion inextricably associated with junk (Christmas, Easter, Halloween, birthdays…) without every adult reiterating the ‘junk makes you feel better’ propaganda every time a child experiences a negative emotion.
I’ve been trying to help people who want to lose weight/have a better relationship with food ever since I wanted to lose weight/have a better relationship with food. The most difficult thing to overcome is working with someone who has believed, for decades, that junk food (and it does need to be junk food – salmon and green beans doesn’t work) will cheer them up/boost morale/alleviate stress – because they have been told this for decades and because – to be honest – it has ‘worked’ for decades. The boss is being unreasonable – reach for a muffin. Teenage tantrums are upsetting – have a cake. A friend seems less friendly – get a box of chocolates. Nurses have just worked the worst shift in their career – 1,500 doughnuts – that should cheer them up.
But it ‘works’ for just a few moments. The sugar gives an almost instant ‘high’ and thus a sense of being cheered up for a truly short period of time – perhaps just a few minutes. Then, likely follows the crash and a low that will make you want another doughnut – not to cheer you up any longer, but to avoid the low that the first doughnut produced. Because it is no accident that doughnuts make you want them…
Processed food
In “Why do you overeat?”, I wrote about one of the fundamental differences between what I called real food and processed food. Real food is naturally predominantly carb/protein or fat/protein. I explained that carb/proteins are things that vegans eat – things that come from the trees and the ground: grains; legumes; fruits and vegetables. Fat/proteins are things that vegans don’t eat – things that come from animals: meat; fish; eggs and dairy products. Fruit is sweet, but not fatty; lamb is fatty, but not sweet. The exceptions, I observed, were nuts and seeds – which have carbohydrate, protein, and fat in decent measures – but no one would describe them as sweet and fatty.
Processed food is a whole different ball game. Fake food manufacturers have worked out that we have not evolved to consume fat and sugar together. Nature has never provided it, but, for some reason, we can’t resist it. Maybe it’s because we evolved to consume as much food as we could lay our hands on – our very survival depended on it. Maybe there’s just something about the combination of fat and sugar that we find irresistible and more’ish.
And nothing is left to chance. I was a board member of Cardiff Metropolitan University for six years. Towards the end of my tenure, a food science lab was built, and the board members were given a tour. I witnessed first-hand the booths where human guinea pigs would sit (often students – perfect place to site a lab) and taste concoctions. The guinea pigs worked hard mind you – lots of questions: how did it look? How did it smell? How did it taste the moment you put it in your mouth? How did it feel in your mouth? How long did it last? How did it feel after you finished it? Then the ‘food technologists’ (don’t even get me started) would add fat, add sugar, change the fat to sugar ratio, tweak the colour, change the consistency and then another version would be passed through the hatch and the guinea pig would answer the same questions all over again. The outcome would be the perfect recipe to be irresistible and more’ish. We want it and we want more of it.
A few of the tweet replies were about free choice – you can always say no to the doughnut. Really? Confession time – I used to work for Mars Confectionery. We had an entire team called “Sales Display.” Their job was to ensure that wherever confectionery was displayed – petrol/gas stations, corner shops, cinemas, grocery stores, clothing shops – the person who impulsively bought confectionery would choose a Mars product and not a Cadbury or Rowntree product. How many purchases are made on impulse? Back then it was 7 out of 10. I doubt that it has changed. Seven out of 10 people walked into a petrol/gas station intending only to pay for their fuel and they walked out with a bar of confectionery.
Back to that nurse, who’s had the worst shift ever, can s/he resist that box of doughnuts? Fat chance! Especially if s/he – like every other human being – has had it reinforced, from the time s/he could crawl, that junk cheers you up. And when you’ve had one? Do you think you won’t want another?
I’ve become acquainted with CrossFit – people and organisation – since the CrossFit Games last August. CrossFit’s health advice is brilliant – “Eat meat and vegetables, nuts and seeds, some fruit, little starch and no sugar. Keep intake to levels that will support exercise but not body fat.” I know a classic CrossFit male, 20s, who follows that advice and looks like one of the competitors. A box of KrispyKreme doughnuts arrived at his workplace one day and ‘G’ was curious and so he tried one. He described the doughnut as “the crack cocaine of the food world.” “I wasn’t even halfway through the first one when I wanted another,” he told me.
If you’re the kind of person who can say no to junk, or have one KrispyKreme doughnut and not want another, you’re probably not overweight or obese. You’re in the minority though – 29% of adults in England are obese; a further 36% are overweight but not obese (Ref 5). The UK is higher still; the US is higher again.
Obesity & overweight among NHS workers
Sticking with England, healthcare workers are similar in terms of obesity. A 2017 paper published in the BMJ reported that 25% of nurses were obese and a further 36% overweight (Ref 6). Other health-care professionals (defined as doctors, pharmacists, dentists, therapists) had lower rates – 14% obese and 35% overweight, but not obese. Unregistered care staff had the highest rates – 32% obese and a further 33% overweight, but not obese. The paper reported that “a systematic review of the impact of personal health behaviours on health promotion practice found that patients are more likely to accept advice offered by a visibly healthy healthcare professional compared with a healthcare professional who is overweight or obese.” The weight of healthcare workers thus has a profound effect on the weight of the nation.
In July 2014, the Chief Executive of the NHS, Simon Stevens, announced plans to introduce incentives to help to “slim down” NHS staff after discovering that 700,000 of his 1.3 million NHS staff were overweight or obese – 300,000 obese and 400,000 overweight. Simon Stevens thought that NHS staff should be setting an example for patients (Ref 7). The story was reported factually in the Nursing Times (Ref 8). There was no mention of fat shaming. I have seen no evidence that the 2014 numbers have gone down. If anything, they will have gone up, alongside national data.
BMI & mortality
Researchers have been studying the association between BMI and mortality for many years. A classic paper from 2005 reported that, relative to those in the normal weight BMI category, those with a BMI above 30 were associated with approximately 110,000 excess deaths across the US and the underweight were associated with approximately 34,000 excess deaths. Interestingly the overweight BMI category (25-<30) was associated with 86,000 fewer deaths (Ref 9). Being overweight, but not obese, was actually better for mortality, but the paper couldn’t bring itself to admit this.
The same lead researcher, Flegal, revisited the data in 2013 and found the same (Ref 10). This time, the results were presented as risk ratios (HRs), not excess deaths. The paper split BMI into the usual categories: overweight (BMI of 25-<30) and obesity (BMI of ≥30). It then further split obesity into class 1 obesity (BMI of 30-<35); class 2 obesity (BMI of 35-<40) and class 3 obesity (BMI 40 or higher). Relative to the normal BMI category, those in the overweight (but not obese) category fared better (again), those in any obesity category fared worse and those in the highest obesity category fared worst of all. (Ref 11).
A 2017 paper referenced both Flegal studies and explored why obesity might have an impact on mortality (Ref 12). Comorbidities covered included type 2 diabetes, oxidative stress, cardiovascular disease, kidney disease, non-alcoholic fatty liver disease, airway impairment (sleep apnoea or daytime distress), PCOS, gastroesophageal reflux, cancer, and restricted movement. (By the way, I have never considered obesity per se to be a disease. As I said in this 2013 post: “I do not think that almost a third of British people have become diseased overnight. I think that obesity is a natural response to an unnatural diet” (Ref 13).
These serious comorbidities aren’t immediate, however. They certainly aren’t immediate enough for most people to change behaviour. We don’t want to be obese; we really don’t, but the immediate desire to have that exquisitely engineered doughnut overrides our bigger desire to be slim at that moment of choice. There are other physical and psychological things going on (which was what “Why do you overeat?” was about) but the immediate gain invariably wins against the longer term pain.
COVID-19 has changed this.
BMI & COVID-19
COVID-19 has brought an immediacy to the notion that obesity can be life threatening. The stark reality right now is that we are living among a virus that has been shown to have the capacity to disproportionately harm people with a high BMI. This is not the slow, but premature, death of type 2 diabetes. This is a young nurse working in ICU one week and dying a few days later. I think that we will look back on our reaction to COVID-19 and realise that we overprotected those who needed no protection and under protected those who needed the most.
The earliest paper I found suggesting a link between metabolic syndrome and COVID-19 was dated March 10th (Ref 14). On March 27th, the World Health Organization issued an “Obesity and COVID-19 policy statement” (Ref 15). Here’s a quotation from the opening: “Based on emerging data and the patterns of infection we have seen in other viral infections, overweight and obesity are also likely to be risk factors for worse outcomes in those who are infected by COVID-19. In the UK, a report suggests that two thirds of people who have fallen seriously ill with coronavirus were overweight or had obesity.” Arguably, from no later than that date, we should have known that obesity was a risk factor and protected people accordingly.
On April 1st, the Obesity Society published an editorial noting the connections between obesity, comorbidities, and the severity of, or death from, COVID-19 (Ref 16). This editorial noted that “Americans have a high burden of Class 3 obesity, with 9.2% of the population with a BMI > 40. This has serious implications for our healthcare system.” This should have warned the US then that it was in for a tougher ride than China.
Since then, the data continue to emerge. As of today, May 9th, there are 81 articles in the academic database, pubmed, about COVID-19 and obesity and they are rising by the day.
In this post (Ref 17), published on April 20th, I reviewed the first paper to use multivariable logistic regression to not only identify, but to prioritize, risk factors (Ref 18). This paper reviewed data from 4,103 patients with lab-confirmed COVID-19 who were treated at an academic medical centre in NY City between March 1st and April 2nd. The patients were reviewed according to whether or not they were hospitalised and how critical they became if hospitalised (critical included ICU/ventilator/hospice/death). Compared with those with a BMI under 30, those with a BMI over 40 were 6 times more likely to be hospitalized. Of those hospitalized, those with a BMI over 40 were 1.7 times more likely to become critical. If we add in ethnicity as a separate risk factor, the NY paper also revealed that those of Asian ethnicity were almost twice as likely as white people to become critical.
The most recent (UK) paper, published as a pre-print (not yet peer reviewed) as I was writing this note, examined the electronic health records of 17 million adult NHS patients to assess factors associated with COVID-19 related deaths in hospital (Ref 19). This paper reported that, compared to those not obese (BMI <30), having a BMI over 40 had an increased risk of dying of more than double (fully adjusted HR 2.27, 95% CI 1.99-2.58). This paper also reported that, compared to people with ethnicity recorded as white, black and Asian people (analysed separately) both had approximately 1.7 times the risk of dying.
I’ve added ethnicity into the discussion for good reason. The final issue to add is viral load. A paper published in the BMJ on May 6th reported “Although the evidence is limited, high infection rates among health workers have been attributed to more frequent contact with infected patients, and higher viral load —the size of the infecting dose of virus” (Ref 20).
So now we have the perfect storm for some healthcare workers – ethnicity, BMI > 40 and exposure to substantially greater viral load than the person who touches a handrail on public transport. Now please observe the photos of the first 100 healthcare workers who died in the UK, in an objective and scientific way (Ref 21). Please look without judgement for possible ethnicity or possible obesity. Please do so as if the lives of those people were your personal responsibility. Now ask yourself, if we knew even a few weeks ago what we know now, would all of these people have been put on the front line, or would any of them have been shielded? They died protecting us. Did they die because we failed to protect them?
References
Ref 1: https://twitter.com/RoyalFreeNHS/status/1252576924628631557
Ref 2: https://twitter.com/DrAseemMalhotra/status/1252861958652452864
Ref 3: Kearns et al. Sugar Industry and Coronary Heart Disease Research. JAMA. 2016. https://jamanetwork.com/journals/jamainternalmedicine/article-abstract/2548255
Ref 4: Harcombe Z. Designed by the food industry for wealth, not health: the ‘Eatwell Guide’. BJSM. 2016. https://bjsm.bmj.com/content/51/24/1730 https://bjsm.bmj.com/content/51/24/1730
Ref 5: https://commonslibrary.parliament.uk/research-briefings/sn03336/
Ref 6: Kyle et al. Obesity prevalence among healthcare professionals in England: a cross-sectional study using the Health Survey for England. BMJ Open. 2017. https://bmjopen.bmj.com/content/7/12/e018498
Ref 7: “Weight’s up Doc: Fat medics told to slim by NHS chief” The Sun. 30 July 2014. https://www.thesun.co.uk/archives/health/1008222/weights-up-doc/
Ref 8: https://www.nursingtimes.net/clinical-archive/public-health-clinical-archive/overweight-nursing-and-medical-staff-should-slim-says-nhs-chief-30-07-2014/
Ref 9: Flegal et al. Excess deaths associated with underweight, overweight, and obesity. JAMA. 2005. https://www.ncbi.nlm.nih.gov/pubmed/15840860
Ref 10: Flegal et al. Association of All-Cause Mortality With Overweight and Obesity Using Standard Body Mass Index Categories. JAMA. 2013.https://jamanetwork.com/journals/jama/fullarticle/1555137
Ref 11: The precise numbers were: Relative to the normal BMI category the HR for being in the overweight category was 0.94 (95% CI, 0.91-0.96), the HR for being in any obesity category was 1.18 (95% CI, 1.12-1.25), the HR for grades 2 and 3 obesity was 1.29 (95% CI, 1.18-1.41)
Ref 12: Abdelaal et al. Morbidity and mortality associated with obesity. Ann Transl Med. 2017. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5401682/
Ref 13: https://www.zoeharcombe.com/2013/06/is-obesity-a-disease/
Ref 14: Gupta et al. Clinical considerations for patients with diabetes in times of COVID-19 epidemic. Diabetes Metab Syndr. 2020. https://www.ncbi.nlm.nih.gov/pubmed/32172175
Ref 15: https://www.worldobesity.org/news/obesity-and-covid-19-policy-statement
Ref 16: Ryan et al. COVID 19 and the Patient with Obesity – The Editors Speak Out. Obesity. 2020. https://onlinelibrary.wiley.com/doi/full/10.1002/oby.22808
Ref 17: https://www.zoeharcombe.com/2020/04/covid-19-risk-factors/
Ref 18: Petrilli et al. Factors associated with hospitalization and critical illness among 4,103 patients with Covid-19 disease in New York City. In pre-print. April 11th, 2020. https://www.medrxiv.org/content/10.1101/2020.04.08.20057794v1
Ref 19: The OpenSAFELY Collabrative. OpenSAFELY: factors associated with COVID-19-related hospital death in the linked electronic health records of 17 million adult NHS patients. PRe-print. 2020. https://www.medrxiv.org/content/10.1101/2020.05.06.20092999v1
Ref 20: Little et al. Analysis Reducing risks from coronavirus transmission in the home—the role of viral load. BMJ. 2020. https://www.bmj.com/content/369/bmj.m1728
Ref 21: https://www.bbc.co.uk/news/health-52242856






What would the response have been if a consortium of local farmers got together and decided to donate a couple hundred pounds of premium Porterhouse steaks to be barbecued in the hospital parking lot for the benefit of the hospital workers? PETA would be demonstrating on one side of the parking lot, claiming you were subjecting the hospital workers to cancer risk, CHD, and of course, type II diabetes, not to mention degrading the climate, along with animal torture. You would need the local police department just to corral the press coverage. But, the really disgusting reaction here would be that the hospital staff would grab the doughnuts before they would ever eat the beef. Note that the cost of the doughnuts was subsidized and thereby far less than the cost of the box that they came in. Forget the cost of the advertising and that Krispy Cream trademark.
The farmers would be accused of trying to kill the hospital staff, and the hospital administration would be pilloried for having allowed such an event. At this point, after ten years of being interested in this topic from a public health standpoint, I can say without reservation that I have wasted my time. I am a tiny minority, and Krispy Cream won, and will keep on winning. I have yet to see one article in the MSM that even remotely resembles the issues outlined here relative to the Coronavirus. If you even hint at an association between this global pandemic and the nature of the food supply, and are a public figure, you won’t survive ten minutes.
Hi Zoe, wow powerful stuff here. I completely agree. I have a 3 year old daughter and I’m very conscious not to use ‘junk’ as a treat. I tell her it’s not good for her…does that upset her?..nah! Cuddles, extra bedtime stories etc work better anyway.
This recent crisis has exposed so much about the nation’s health. However I can’t help wonder what evil machinations the fake food industry are already plotting to ensure their addicted customers still keep buying their stuff.
I also note vegans have gone awfully quiet about how animals cause carbon emission problems…
Please keep up the good work xx
Zoe,
As always a great and insightful presentation of the facts. I always look forward to your weekly posts.
I will be sharing this. You are going to be saving lives again.
Thanks,
Brett
Cancer research also came under massive criticism for fat shaming from its campaign on obesity in 2019. According to an editorial in the lancet ‘an open letter from more than 60 researchers, public health professionals and dietians to stop the advertisements with an online petition. My BAME colleagues are very aware and frightened of catching Covid19 . Most are obese and admit it openly. Office full of cake s and biscuits ( extra boost to sugar mountain to celebrate day of the midwife last week).Our office is shared by a minimum of 10 People and impossible to social distance, we have to share a computer and office phone between 3 to 4 staff. Pregnant colleagues are organised to work in their own office and have telephone contacts only or have gone sick with stress. The system is so unfair to my very at risk BAMEcolleagues. I applaud Aseem Malhotra for his tenacity to follow his principles but fear we have a very long battle ahead. On a positive Covid 19 has been the catalyst for my partner with uncontrolled Type 2 DM to completely change his diet, he eats real food and no sugar. Lost lots weight around his waist and looks & feels healthier l. Zoe thank you for your excellent weekly newsletter and analysis of the research. Looking forward to next week.
Hi Zoe,
I think it’s vitally important not get drawn into others narratives from the get-go. It’s not fat-shaming, but it is diet enlightening. However, maybe you could find a better riposte? Bye the way, I just love your work and your rat-a-tat delivery! Keep kicking the door in!!
Cheers,
Shaun
Thank you once again!
Especially Ref21 sums it up!
Hi Zoe,
(We met in Tel Aviv at the Metabolix conference and you gave me a copy of your PhD!) I’ve been LCHF for 18+ years, originally went down from 17 stone to 10 stone (upper end of normal for my height), then pregnancy led to a gradual regain of quite a lot of that weight despite remaining LCHF, then a few years later when I added in intermittent fasting I lost a lot of it again, but unfortunately still not back down to where I was. So now (47 yrs old) I am still classified as overweight. It’s been a while since I got on a scale but I’m probably in the middle of the overweight BMI category. However, I almost never eat sugar or starches (maybe 4 or 5 meals a year), I never eat anything processed, my bloodwork is excellent and when I did a dexa scan a couple years ago I had almost no visceral fat. With that background – still lots of subcutaneous fat, but hourglass figure and healthy metabolism – do you think I’m still at higher risk for covid-19 with what you’ve read, simply for having the excess subcutaneous fat? Or is it that the excess fat usually correlates to underlying metabolic diseases, and since I have avoided those by eating well, I should have ‘normal’ risk rather than elevated? What are your thoughts?
Thank you!
Deborah
Hi Deborah
I remember you well! The article (and evidence) notes that overweight, but not obese, was actually the best category to be in. This had lower mortality associated with it than even the normal weight BMI. I think this is because it is still the case that age is the massive determinant of death and some illnesses can cause elderly people to lose weight rapidly and – if they have nothing to lose – they’re in big trouble.
It happened to my mum – she had a burst appendix, which had got really bad before it burst and before she was rushed to hospital. She was in hospital for a couple of weeks and lost about 7kg during the whole pain/operation/recovery period. She probably had about 10kg to lose, so she was fine. Remember Cheryl Cole who got Malaria and nearly died? She had nothing to lose – can be bad for young people too.
It sounds like you’re doing really well – good bloods, good scan, avoiding sugar and starch – there are papers being written on metabolic health and COVID-19 (see Ref 14 above as the first I found) but that doesn’t sound like where you’re at.
Hope you’re doing well generally in these strange times.
Best wishes – Zoe
Zoe, thanks – we’re doing relatively well, although since my husband teaches foreign students he is on unpaid leave for who knows how long… Israel has handled everything pretty well and we have a very low death/sickness rate. My parents who are in their mid-late seventies in London are thankfully healthy and avoided infection and are staying home, although they’ve lost friends to covid. I’ve had my kids home now for nearly two months and the 7 year old went back to school last week, 11 year old still home. It’s certainly been interesting, and when we were in strict lock down it was pretty difficult – we don’t have a garden, we’re in an apartment in the city. Now it’s easier.
My husband is tall and slim and basically eats the way I do, but with desserts a couple of times on the weekend. When this all started, he’d been skipping breakfast for a few months (on my advice) and he’d lost the very few pounds he’d put on around his middle. I told him I thought he should start eating three meals again precisely so that if he got ill, he’d have some fat stores to tide him over! He’s almost 6’2″ and only about 11.5 stone.
I hope you are staying well too! Thanks for everything you do!
Deborah