Keto diet under attack

Executive summary
* A paper was published in July 2021 entitled “Ketogenic Diets and Chronic Disease: Weighing the Benefits Against the Risks.” It concluded that the risks of the diet outweighed the benefits.
* The paper was a narrative review – not a trial or study. The review was authored by plant-based diet advocates.
* The review started with the premise that fruit, vegetables, whole grains, legumes and fiber are healthy and thus ketogenic diets can’t be healthy because they’re not based on these. That claim is not evidence based.
* The paper concluded that ketogenic diets can help with drug-resistant epilepsy – the drug resistant caveat is not needed.
* The paper concluded that ketogenic diets can induce weight loss but that meta-analysis has not found a substantial difference in weight loss vs low-fat diets. This is correct, although the emerging Virta evidence (one trial, not meta-analysis) is promising.
* In the diabetes section, the paper concluded that "Ketogenic diets depress appetite, promote weight loss, reduce blood glucose values, and decrease HbA1c in the short term" and that "diabetes medications are frequently reduced or eliminated." This is correct.
* The section on non-alcoholic fatty liver disease (NAFLD) contained nothing of relevance to ketogenic diets. The conclusion on cancer was that “large, well-designed, randomized clinical trials are needed to determine the safety and effectiveness of ketogenic diets in cancer treatment.” This is correct.
* The conclusion on Alzheimer’s Disease was under-reported. Evidence for ketogenic diets being of benefit for Alzheimer’s is emerging currently with four relevant systematic reviews/meta-analyses published in 2020-2021.
* The paper claimed harm from ketogenic diets for cardiovascular disease (CVD), kidney health and pregnancy, but these sections did not cover ketogenic diets. They were about low-carbohydrate diets or high animal protein diets at best and even then the claims did not withstand scrutiny.
* The paper struggled to be positive about ketogenic diets – probably because of the plant-bias of the authors and their organisations. Even the positive evidence for ketogenic diets in the paper was played down and accompanied by unnecessary caveats.
Introduction
I received six emails about this week’s note – that might be a record – so it became an obvious one to review. It was covered more in the US than the UK. New Atlas reported the story with the headline "Concerns raised over long-term health risks of ketogenic diets" (Ref 1). Eat this not that web site reported "This Popular Diet Is a Health ‘Disaster,’ Says New Study" (Ref 2). Yahoo Life went with "‘The keto diet is a disease-promoting disaster’: The eating plan raises cholesterol, hastens kidney failure and is unsafe in pregnancy" (Ref 3). Science blog reported “Review Finds Keto Diet Ups Heart Risks, Cancer Risk, Dangers To Pregnant Women And Kidney Patients” (Ref 4).
The headlines came from an article written by Crosby et al, in Frontiers in Nutrition, which was published on July 16th, 2021, entitled “Ketogenic Diets and Chronic Disease: Weighing the Benefits Against the Risks” (Ref 5). The lead author and four others were from the Physicians Committee for Responsible Medicine (a plant-based diet organization). Another author was from Loma Linda University – another plant-based diet organization. The senior author, Neal Barnard, is a well-known vegan.
For my declarations of interest, I don’t follow a ketogenic diet; I never have. I don’t recommend (or not recommend) one. The diet books I write are about real food rather than low carbohydrate intake (although when people ‘choose that real food for the nutrients provided’ – my second principle – they will naturally choose low-carb foods). I think that some people do well on a ketogenic diet but not all people. We get a number of keto followers joining our forum and the high fat bit of low carb high fat has been overdone and has not been helpful for them. I think ketogenic diets should be tried, if not followed, for epilepsy and seizure disorders. I think people with diabetes (type 1 or 2) will benefit from minimising carbohydrate intake. However, some people struggle to stick to ketogenic levels of carbohydrate and yet they can still achieve significant improvements with low-carbohydrate diets and thus broader options can be embraced. Those are my confirmation biases going into this review.
The definition of keto
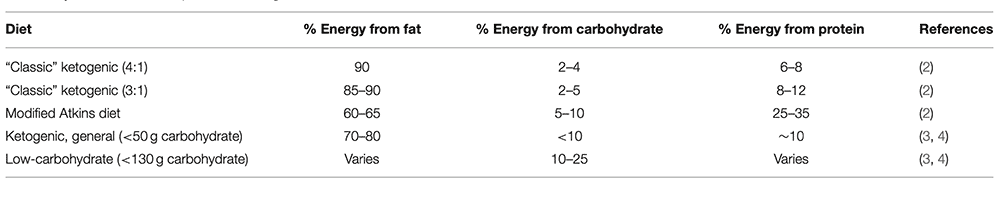
In Table 1, the article set out the definitions it planned to rely on:
The Noakes/Windt paper defined low-carb high-fat (LCHF) diets as follows (Ref 6):
▸ Moderate carbohydrate diet (26–45% of daily kcal)
▸ LCHF diet (<26% of total energy intake or <130 g CHO/day)
▸ Very LCHF (ketogenic) diet (20–50 g CHO/day or <10% of daily kcal of 2000 kcal/day diet)
The Noakes/Windt paper does not specify protein intake. Ketogenic diets are defined in that paper by carbohydrate level, not by protein intake. I had not previously seen the top two definitions of “Classic” ketogenic diets – 4:1 or 3:1 – in Table 1 of the Crosby et al paper. The paper described these two diets as “generally medically supervised” and specifically for epilepsy. Reference 2 in the Crosby et al paper was given for both definitions and it was about “modified ketogenic diets for the treatment of epilepsy”. Those two diets can be ignored for the general review, therefore. The protein intake in the three diets in Table 1 with the word “ketogenic” in the title all seemed low in protein. Definitions are everything when we’re talking specific diets.
Line 4 in Table 1 – ketogenic general (<50g carb and <10% energy from carb) concurs with the Noakes/Windt definition of a ketogenic diet. Line 5 in Table 1 (<130g carb and <26% energy from carb) also concurs with the Noakes/Windt definition of a LCHF diet, but we’re not reviewing low-carb diets, we’re reviewing ketogenic diets. We need to stay in the territory of a genuine ketogenic diet (i.e., <50g carb and <10% energy from carb) as we explore this paper, therefore.
The paper
The paper is a review paper. It was not a trial, or an epidemiological study, or a systematic review (looking at all evidence), or a meta-analysis (pooling together all evidence). It was a narrative review. This means that the authors don’t have to look at all the evidence (although they should). They can cherry pick papers that suit their argument and they can have an agenda (although they shouldn’t). To be fair, the authors do seem to have tried to find systematic reviews and meta-analyses wherever possible to examine the best available evidence.
The paper was structured with an opening section on diet quality and then subheadings for different conditions. The conditions covered were seizure disorders, obesity and weight, diabetes, non-alcoholic fatty liver disease (NAFLD), cancer, Alzheimer’s disease, cardiovascular disease (CVD), kidney health, pre-pregnancy and pregnancy. We’ll examine the paper’s claims for each area. I’ll number the arguments as they appeared in the paper and provide counters where appropriate or accept the argument if it is evidence based…
Diet Quality
I found the diet quality section quite amusing. The arguments were essentially:
1) Fruits, vegetables, whole grains and legumes are healthy and ketogenic diets don’t include much of these.
The counter argument is that animal foods are healthier and plant-based diets don’t include any of these.
2) “Low-carbohydrate diets are often low in thiamin, folate, vitamin A, vitamin E, vitamin B6, calcium, magnesium, iron, and potassium.”
The counter argument is that this claim was made on the basis of one bizarre interpretation of an ‘Atkins’ diet in a 2001 paper, which has nothing to do with a typical ketogenic diet.
First sight of this claim surprised me because plant-based diets are the ones deficient in key nutrients. Diets that exclude animal foods do not provide retinol, B12, D3, heme iron and omega-3 fatty acids in the form we need them (DHA and EPA). I thus checked the source for this claim and it was reference 9 in the Crosby et al paper (Ref 7). Their reference 9 is a paper by Freedman, King & Kennedy. I am very familiar with this paper, having analysed it in detail for my 2009 obesity book. The analysis can be seen here (Ref 8). The nutrient deficiencies claimed were entirely for the Atkins diet. However, it wasn’t even the Atkins diet – it was what low-fat/low-calorie people might think the Atkins diet is.
The diet presented as most nutritionally deficient by Freedman, King & Kennedy was (based on) the Atkins induction diet. The calorie intake for this diet was given as 1,152, which is absurd. The whole point of the Atkins diet is to eat low carb foods to satiety. The diet for one day was described as comprising eggs (2), bacon strips (3), cheeseburger (4oz), steak (4oz), shrimp salad (1.5 cups), 1 cup sugar-free jello & 1 tablespoon sugar free cream. That is a world away from the real Atkins diet, let alone the keto diet that I see people consume (eggs, nose to tail cuts of meat (including offal), oily fish, cheese, greens, some nuts and seeds), which provides all nutrients needed and in the form needed. This was a disingenuous selection of an old paper (2001), with an absurd notion of what the Atkins diet is (1,152 calories), notwithstanding that the macronutrient ratios of 60% fat, 35% protein and 5% carbohydrate are not within either the Noakes or Crosby et al definitions of a ketogenic diet.
This claim is non-sense and should be ignored.
3) Ketogenic diets are typically low in fiber and fiber is wonderful (paraphrased!)
I have countered this many times in many ways:
i) Ketogenic diets can be just as high in fiber as carb heavy diets (Ref 9).
ii) Not that fiber is anything to get excited about (Ref 10).
Epilepsy & seizures
4) “Drug-resistant epilepsy can reduce seizure frequency by at least 50% with a ketogenic diet.”
No need to counter this – except that the “drug-resistant” caveat is not needed.
This was a short section in the paper, which reached that conclusion. The paper clarified: “According to a 2018 Cochrane Review, most affected individuals can eliminate seizures with medication, but about 30% cannot.” The authors added that “long-term adherence is challenging”, which I suspect it is, but it’s important to recognise the power of a ketogenic diet for people with seizure disorders. Plus, it did seem a bit churlish to add a caveat to the key part of the paper where there was (what felt like reluctant) acceptance of the value of a ketogenic diet.
Obesity & weight management
5) Ketogenic diets can induce weight loss, but results are not very different to weight loss achieved with low-fat diets.
No need to counter this.
The first paper cited to support this examined a meta-analysis of “38 studies lasting 6–12 months and including 6,499 participants, of low-carbohydrate diets, defined here as <40% of energy from carbohydrate” (Ref 11). We can ignore that, as it’s not a meta-analysis of ketogenic diets (Ref 12). The second paper cited was relevant – the Bueno et al 2013 meta-analysis of randomised controlled trials (lasting at least one year) comparing ketogenic diets with low-fat diets (Ref 13). Bueno et al found that ketogenic diets led to marginally more weight loss than reduced-fat diets (less than 1kg) and that there was no statistically significant difference in weight loss in the trials that followed people for at least 2 years.
Attention was then given by the Crosby et al paper to the Dr Kevin Hall papers (Ref 14). We have covered these before (Ref 15).
The Virta study has provided valuable data in this subject area since approximately 2018. Some of this work was included in the references for the diabetes section in the Crosby et al paper, but not in the obesity/weight section. The Virta trial examines ketogenic diets and has data recorded and reported for weight loss and HbA1c for one year and two year time scales. The 1 year average weight loss was 14.3kg and the 2 year average weight loss was 11.9kg, indicating some regain, on average (Ref 16). This compared very favourably with usual care. I compared the results against the very low-fat/very low-calorie DiRECT study and Virta still compared favourably. All summaries are in this post (Ref 17).
The Virta research has the benefit of involving patients with high motivation to adhere to a ketogenic diet (obesity and type 2 diabetes). Patients could choose to be in the intervention or not and thus it can be assumed that only those who really wanted to follow a strict protocol would start the program. This will likely have made the results better than in a randomised trial.
The Virta trial is one study. The Crosby et al authors were right to focus on systematic reviews and meta-analyses comparing many trials of low-fat diets with ketogenic diets (ignoring low-carb, but not ketogenic, diets). The evidence from such papers does not make a compelling case for ketogenic diets. There is weight loss, but it is not dramatically different to that achieved on low-fat diets. Ketogenic diets may be powerful, but meta-analysis evidence does not currently support this claim.
Diabetes
6) There’s not much evidence for ketogenic diets and type 1 diabetes; there’s some good evidence for ketogenic diets and type 2 diabetes.
No need to counter this.
Type 1 diabetes and type 2 diabetes were covered separately in this section. There is virtually no evidence for ketogenic diets and type 1 diabetes. I searched the academic database, pubmed, and found the same. There is a surprising dearth of research in this important area. The Crosby et al paper cited three references acknowledging that a ketogenic diet can improve blood glucose control while cautioning that hypoglycaemic episodes may be more frequent – which they will be unless insulin is reduced to match the reduced need for it.
The type 2 diabetes section cited nine references (including some work of Drs Eric Westman, Sarah Hallberg, Laura Saslow etc) and opened with the passage “Ketogenic diets depress appetite, promote weight loss, reduce blood glucose values, and decrease HbA1c in the short term.” This section closed with the passage “In other clinical trials with ketogenic diets, diabetes medications are frequently reduced or eliminated… Few additional negative impacts on global measures of health have been reported in short-term studies on type 2 diabetes. Long-term effects have not been elucidated.”
There was some criticism of ketogenic diets for type 2 diabetes in between these two positive passages – the paper did read as if it struggled to say anything positive about ketogenic diets for more than a couple of lines before having another ‘pop.’
NAFLD
7) “Lifestyle modifications, particularly diet change, weight loss, and exercise, are the primary modality for treating NAFLD.”
No need to counter this, but it makes no specific statements about ketogenic diets.
This section contained one reference (their ref 63) about ketosis “It has been suggested that achieving ketosis may have a benefit in ameliorating fatty liver.” Bizarrely reference 63 did not contain one single reference to ketosis or a ketogenic diet. On the contrary, reference 63 stated “the macronutrient composition [of the diet] is scarcely important as long as calorie restriction is maintained.” This reference can be ignored, as can the rest of the section on NAFLD which offered no specific evidence either way. (If you search ketogenic diets and NAFLD on pubmed, there are no systematic reviews or meta-analyses. There were 35 articles relevant to the subject area ranging from individual trials to review papers.)
Cancer
8) “…large, well-designed, randomized clinical trials are needed to determine the safety and effectiveness of ketogenic diets in cancer treatment.”
No need to counter this.
This section referenced two systematic reviews (Ref 18). One was specifically on brain tumours, the other was on cancer more generally. The conclusion was that evidence is accumulating, but more research is needed. I repeated the search and found one paper that may have been published as the Crosby et al paper was in peer review (Ref 19). This found 39 studies involving 770 patients and found similarly that there was no conclusive evidence for anti-tumour effects or improved survival. This paper concluded "clinical evidence for the effectiveness of ketogenic diets in cancer patients is still lacking." That does seem to be the case.
Alzheimer’s Disease (AD)
9) “In a 2020 review of short term ketogenic diets, 6 of 9 controlled trials found significant cognitive improvements in the intervention groups, while other trials did not.” This was followed with “Saturated fat intake, which typically increases on a ketogenic diet, is strongly associated with AD risk.” What was that observation about not being able to say anything positive for very long?
The counter to this is that this section missed some evidence. I searched pubmed for “ketogenic diets Alzheimer’s” and for systematic reviews and/or meta-analysis and found four papers – only one of which was cited by Crosby et al. Two would likely have been published too late for Crosby et al, but the Grammatikopoulou et al paper “To Keto or Not to Keto? A Systematic Review of Randomized Controlled Trials Assessing the Effects of Ketogenic Therapy on Alzheimer Disease” should have been included. All three of the systematic reviews found positively for the ketogenic diet. One concluded “the studies reviewed confirmed the effectiveness of this diet in improving the cognitive symptomatology of the aforementioned diseases (Alzheimer’s disease, Parkinson’s disease and others)” (Ref 20).
Cardiovascular Disease (CVD)
10) “The effect of low-carbohydrate diets on plasma lipid concentrations is a major concern.”
The counter to this is – if you have any evidence that ketogenic diets cause CVD, please present it; this section was about lipoproteins (mostly low density lipoproteins, but also high density lipoproteins) and not CVD. It was also about low-carbohydrate diets and not ketogenic diets.
Kidney health
11) “The evidence of the renal-specific effects of ketogenic diets is limited but worth noting.” The paper went on to mention kidney stones, development of chronic kidney disease and make other insinuations, which the references didn’t support. The references moved from paediatric epilepsy literature to general papers on red meat or animal protein. Keto diets tend to include red meat and animal protein but a) they don’t have to and b) one can’t leap from allegations against animal foods to claims against a ketogenic diet. Much of my calorie intake daily comes from dairy products, but I don’t follow a ketogenic diet.
The counter to this is – much was implied in this section, but little was claimed and thus there is little to counter. Ignore the inuendo and stick to facts.
Pre-pregnancy and pregnancy
12) “Low-carbohydrate diets followed prior to conception or during the periconceptual period are associated with an increased risk of birth defects and gestational diabetes, respectively.”
This assertion relied entirely on one paper (Ref 21), which I dissected at the time of its publication (Ref 22), including writing a letter to the journal (Ref 23).
We can dismiss the paper swiftly for this Monday note, as it was about a low-carbohydrate diet (c. 95g/day) and not a ketogenic diet. My rebuttal is there for any concerns about low-carb diets and neural tube defects generally. I found this birth defects paper to be a particularly low blow against low carb, as pregnancy is a worrying enough time without claims like this being made.
Conclusion
The closing section of the paper reported adverse effects of ketogenic diets “especially within the first few days.” The paper reported that people might experience fatigue, headache, nausea, constipation, hypoglycaemia, “keto flu” and “brain fog” and indeed they might. Keto sites warn of such things. However, people also report having better energy levels, more even energy levels, reduced food cravings, more stable blood glucose levels, better sleep and so on – once they have adapted to a ketogenic diet.
The paper’s conclusion was (verbatim):
“Ketogenic diets reduce seizure frequency in some individuals with drug-resistant epilepsy. These diets can also reduce body weight, although not more effectively than other dietary approaches over the long term or when matched for energy intake. Ketogenic diets can also lower blood glucose, although their efficacy typically wanes within the first few months.
Very-low-carbohydrate diets are associated with marked risks. LDL-C can rise, sometimes dramatically. Pregnant women on such diets are more likely to have a child with a neural tube defect, even when supplementing folic acid. And these diets may increase chronic disease risk: Foods and dietary components that typically increase on ketogenic diets (eg, red meat, processed meat, saturated fat) are linked to an increased risk of CKD, cardiovascular disease, cancer, diabetes, and Alzheimer’s disease, whereas intake of protective foods (eg, vegetables, fruits, legumes, whole grains) typically decreases. Current evidence suggests that for most individuals, the risks of such diets outweigh the benefits.”
I think that a fairer conclusion would be:
Ketogenic diets, if based on animal foods (as they usually are) are naturally optimally nutritious – including the nutrients we need and in the form that we need them. Ketogenic diets can reduce or even eliminate seizures. The Virta study is one of the first to provide large and longer-term data for ketogenic diets and this provides good evidence for weight loss and HbA1c improvements at one and two years. Meta-analysis currently available of several trials of ketogenic diets vs low-fat diets does not show compelling differences. There is some good evidence for ketogenic diets and type 2 diabetes. The diet is so powerful that meds need to be reduced to avoid hypoglycemia (for types 1 and 2). There are no meta-analyses for NAFLD or cancer to support claims for the value of ketogenic diets. Evidence for ketogenic diets being of benefit for Alzheimer’s is emerging currently with four relevant systematic reviews/meta-analyses published in 2020-2021. No evidence of harm was presented for CVD, kidney health or pregnancy – although plant-biased advocates imply otherwise.
References
Ref 1: https://newatlas.com/health-wellbeing/long-term-health-risks-ketogenic-diets/
Ref 2: https://www.eatthis.com/news-keto-diet-warning-study/
Ref 3: https://uk.yahoo.com/style/keto-diet-a-disease-promoting-disaster-093817706.html
Ref 4: https://scienceblog.com/524530/review-finds-keto-diet-ups-heart-risks-cancer-risk-dangers-to-pregnant-women-and-kidney-patients/
Ref 5: Crosby et al. Ketogenic Diets and Chronic Disease: Weighing the Benefits Against the Risks. Frontiers in Nutrition. July 2021.
https://www.frontiersin.org/articles/10.3389/fnut.2021.702802/full
Ref 6: Noakes & Windt. Evidence that supports the prescription of low-carbohydrate high-fat diets: a narrative review. British Journal of Sports Medicine. 2016. https://bjsm.bmj.com/content/51/2/133.abstract
Ref 7: Freedman, King & Kennedy. Popular diets: a scientific review. Obes Res. 2001. https://pubmed.ncbi.nlm.nih.gov/11374180/
Ref 8: https://www.zoeharcombe.com/2014/08/weight-loss-correlates-with-low-carb-not-low-calorie/
Ref 9: https://www.zoeharcombe.com/2019/01/does-low-carb-mean-low-fiber/
Ref 10: https://www.zoeharcombe.com/?s=fiber
Ref 11: Chawla et al. The effect of low-fat and low-carbohydrate diets on weight loss and lipid levels: a systematic review and meta-analysis. Nutrients. 2020.
Ref 12: The paper reported that more than half of included diets met the criteria for a general ketogenic diet, but then just these studies should have been examined to make statements about a general ketogenic diet.
Ref 13: Bueno et al. Very-low carbohydrate ketogenic diet v. low-fat diet for long-term weight loss: a meta-analysis of randomised controlled trials. Br J Nutr. 2013.
Ref 14: Hall et al. Effect of a plant-based, low-fat diet versus an animal-based, ketogenic diet on ad libitum energy intake. Nat Med. 2021.
and
Hall et al. Energy expenditure and body composition changes after an isocaloric ketogenic diet in overweight and obese men. Am J Clin Nutr. 2016.
Ref 15: https://www.zoeharcombe.com/2020/05/animal-based-low-carb-vs-plant-based-low-fat-diets/
Ref 16: https://www.zoeharcombe.com/2020/09/low-calorie-vs-low-carbohydrate-for-t2d-remission-direct-vs-virta/
Ref 17: https://www.zoeharcombe.com/2020/09/low-calorie-vs-low-carbohydrate-for-t2d-remission-direct-vs-virta/
Ref 18: Martin-McGill et al. The role of ketogenic diets in the therapeutic management of adult and paediatric gliomas: a systematic review. CNS Oncol. 2018
and
Klement et al. Ketogenic diets in medical oncology: a systematic review with focus on clinical outcomes. Med Oncol. 2020.
Ref 19: Römer et al. The use of ketogenic diets in cancer patients: a systematic review. Clin Exp Med. 2021. https://pubmed.ncbi.nlm.nih.gov/33813635/
Ref 20: Pavón et al. Ketogenic diet and cognition in neurological diseases: a systematic review. Nutr Rev. 2021. https://pubmed.ncbi.nlm.nih.gov/33354711/
Christensen et al. Use of ketogenic diets in the treatment of central nervous system diseases: a systematic review. Nord J Psychiatry. 2021. https://pubmed.ncbi.nlm.nih.gov/32757903/
Grammatikopoulou et al. To Keto or Not to Keto? A Systematic Review of Randomized Controlled Trials Assessing the Effects of Ketogenic Therapy on Alzheimer Disease. Adv Nutr. 2020. https://pubmed.ncbi.nlm.nih.gov/32597927/
Ref 21: Desrosiers et al. Low carbohydrate diets may increase risk of neural tube defects. Birth Defects Research. 2018.
Ref 22: https://www.zoeharcombe.com/2018/02/low-carb-diets-birth-defects/
Ref 23: Harcombe. Comments on “Low carbohydrate diets may increase risk of neural tube defects.” Letter to the editor. May 2018. https://onlinelibrary.wiley.com/doi/10.1002/bdr2.1335





Away back in 1961, I was involved in a TV programme in which a group of us were guinea pigs put on different dietary regimes. I was put on a ketogenic regime. I was also fighting (yet again) nicotine addiction. Point being two life time behaviours being challenged simultaneously. It can be done.
after a short time I was nicotine free and considerably healthier at the end of the programme (we were constantly medically assessed.
.
I am not sure whether sugar addiction is worse than nicotine, or other addictive substances, it certainly up there with (gasp) assorted unmentionables.
I am not sticking to a ketogenic diet but I am careful about what carbohydrates I eat and how much.
It is not difficult if you avoid prepackaged “food” from supermarkets.
Hi Peter
That’s really interesting about smoking and diet. It could be argued that trying to address one addiction might open the door to another, but it can also close it I guess!
They say that food is worse because you can’t go cold turkey on it (excuse the pun). You can avoid cigarettes, but you need to eat. The answer, of course is – yes we need to eat, but we can stick to stuff to which we aren’t addicted! I’ve never had cravings for salmon and green beans!
Best wishes – Zoe
Hi Zoë
Insulin is 100 years old, so is Russel Wilder’s experiments with keto for epilepsy. The guy who finalized 4:1 keto was Peterman MG, The Ketogenic Diet, JAMA. 1928;90(18):1427–1429. doi:10.1001/jama.1928.02690450007003
“Classic”.
This was before any pills for these sicknesses t1d and epilepsy, only cure was diet. T2d was to become an issue…
Of course there was no word such as RCT… Of course you would need one to prove old methods useful…NOT.
Hi JR
Many thanks for this – wow – 1928!
Best wishes – Zoe
Cholesterol is found in atheroma, therefore eat less cholesterol, or saturated fats, or animal fats, as long as you eat more Vegan.
Calcium is found in atheroma, therefore go on a low calcium diet. That’s nonsense, of course, but so is the first sentence.
Hi Zoë, i am a bit confused.
In section 5, Obesity & weight management, “Ketogenic diets can induce weight loss, but results are not very different to weight loss achieved with low-fat diets.” Your response is “No need to counter this.” PHC UK has a summary of RCT studies comparing low carb to low fat for weight loss that concludes that low carb is a clear winner, 36 to 0, when the results are statistically significant.
Can you help me understand the difference between the 2 positions?
https://phcuk.org/wp-content/uploads/2021/02/Summary-Table-Of-Randomised-Controlled-Trials-Comparing-Low-Carb-To-Low-Fat-Diets-09.02.2021.pdf
Jacques
Hi Jacques
Good question – I checked the PHC list before making that statement and it’s title is “A summary table of randomised controlled trials comparing low-carb diets of less than 130g carbohydrate per day to low-fat diets of less than 35% fat of total calories compiled by the Public Health Collaboration.”
It’s not a summary of ketogenic diets vs low fat diets therefore.
I meant to put a p.s. on the note that I’m really open to any evidence on ketogenic diets that I may have missed but I only searched for keto diets as that was the title of the paper and that was the arena that we were supposed to be sticking to – hence why I pointed out when the paper didn’t.
I hope this helps
Best wishes – Zoe