Meat guidelines – the evidence

Executive summary
* Six papers about red and processed meat were published in the Annals of Internal Medicine on 30th September 2019. The first was a summary paper about dietary guidelines. The second was a systematic review of randomised controlled trials. There were three systematic reviews and meta-analyses of cohort (observational) studies and one final paper on attitudes towards eating meat.
* The summary recommendations were that adults should continue current unprocessed and processed red meat consumption, although the recommendations were reported as weak and based on low-certainty evidence.
* The summary paper noted that current guidelines are based on observational studies and that these cannot establish causation; they don’t report absolute differences; and they are at high risk of confounding (e.g. the healthy person confounder).
* The paper examining randomised controlled trials (RCTs) reported that there were no significant findings for intake of any kind of red meat from the 12 studies that met their criteria. The unreported issue was that none of the RCTs changed one thing alone. Most changed fat intake, fruit and veg intake, grain intake, and the meat intake also just happened to be different. No RCT did change meat alone. No RCT can change meat alone. If any differences had been observed, it would not have been possible to say that they were due to differences in meat intake and not the multiple other things that changed.
* The three systematic reviews and meta-analyses of cohort studies examined tens of studies, involving millions of people, followed for up to 34 years. The data are vast. The quality of the data was reported as low or very low throughout.
* The sixth paper, on attitudes to meat eating, found that omnivores are generally unwilling to change their meat consumption – and there is little point developing dietary guidelines that will be ignored.
* The paper has sparked hostile reactions (e.g. from the Physicians Committee (Ref 1) and the True Health Initiative) and there has already been a demand for the papers to be retracted. Those who live by nutritional epidemiology don’t like it being used against them.
* An editorial in the Annals of Internal Medicine suggests that retraction demands will be rejected. The six papers were seen as comprehensive in the data examined and consistent in their cautions.
Introduction
Last week’s note was all about the dietary guidelines for dairy products being wrong. On the same day that it was published, the New York Times reported that the advice to eat less meat has been wrong all along: “Eat Less Red Meat, Scientists Said. Now Some Believe That Was Bad Advice” (Ref 2). The story made headlines worldwide (Ref 3).
The headlines came from six papers, which were published in the Annals of Internal Medicine. The papers were written by a collaboration of several international authors. A panel of 14 members from 7 countries voted on the final recommendations. Strict criteria limited the conflicts of interest among panel members (although this was soon questioned by the media (Ref 4)). The recommendations were developed using the NutriRECS process, which included rigorous systematic review methodology and GRADE methods to rate the certainty of evidence and to develop recommendations from that evidence (Ref 5).
The first paper “Unprocessed red meat and processed meat consumption: dietary guideline recommendations” reported that the papers were focused on meat and nutrition – considerations of environmental impact or animal welfare did not influence the recommendations (Ref 6).
The summary recommendations were: “The panel suggests that adults continue current unprocessed red meat consumption (weak recommendation, low-certainty evidence). Similarly, the panel suggests adults continue current processed meat consumption (weak recommendation, low-certainty evidence).” i.e. no change was recommended from current intake, but the evidence for any recommendations was weak.
Accompanying the paper on dietary guidelines were four systematic reviews addressing the health effects associated with red meat and processed meat consumption. The sixth paper reviewed people’s health-related values and preferences regarding meat consumption. For those who want to read the full articles, links to all six papers are in the references. I’ve picked out the key points below:
Paper 1 – dietary guidelines (Ref 3)
This paper opened by noting that the 2015-2020 Dietary Guidelines for Americans recommend limiting red meat intake, including processed meat, to approximately one serving per week. The UK guidelines were noted as limiting the intake of both red and processed meat to 70 grams/day. Paper 1 immediately cautioned that these recommendations are based on observational studies. Then the three fundamental flaws of epidemiology, which I reiterate in every article about observational studies, were listed: these studies cannot establish causation; they don’t report absolute differences; and they are at high risk of confounding. You can’t imagine how joyful it was to read that on the first page of an academic paper.
The panel considered all-cause mortality, major cardiometabolic outcomes (cardiovascular mortality, stroke, myocardial infarction, and diabetes), cancer incidence and mortality (gastrointestinal, prostate, and gynecologic cancer), quality of life, and willingness to change unprocessed red or processed meat consumption as “critically important” for developing recommendations.
The panel reviewed any randomised trials available, as well as cohort studies with 1,000 or more adults. Panellists considered 3 servings per week as a realistic reduction in meat consumption to examine e.g. moving from 7 to 4 servings or 4 to 1 servings. The average current intake was reported as 2-4 servings per week in North America and Western Europe (I was surprised it was that low).
Paper 2 (Ref 7)
Paper 2 was arguably the most important, as it was the one reviewing randomised controlled trials and not observational studies. (RCTs can establish causation). However, even a cursory review of the study selection and the “Table of studies” included would confirm that this paper is not robust. It may be the best evidence we have, but it’s not robust.
Studies were included if the intervention and control diets differed in meat intake by at least 1 serving per week. The abstract of Paper 2 noted that “Of the 12 eligible trials, a single trial enrolling 48,835 women provided the most credible, though still low-certainty, evidence that diets lower in red meat may have little or no effect on all-cause mortality, cardiovascular mortality, and cardiovascular disease.” This tells us that the Women’s Health Initiative was the most credible study found. This was undertaken exclusively on menopausal women (and so is not generalisable to whole populations) and the diet involved multiple changes including reducing total fat to below 20%, increasing fruit and vegetable intake to more than ≥ 5 servings and grains to ≥ 6 servings daily. How can any differences observed be claimed to be the result of meat intake?
Another study involved 85 people adopting a Mediterranean diet (olive oil, vegetables, fruit, whole grains, nuts, legumes, fish and < 1 serving of meat a week) vs 81 people continuing their normal diet to act as the control. Another study involved 17 people adopting a high carb/meat once a week diet and 16 people adopting a high protein/meat four times a week diet. In every one of the 12 studies, how can it be claimed that the difference in meat consumption was responsible for any differences observed when so many things changed?
This paper produced a “Summary of findings” table. This reported that there were no significant findings for intake of any kind of red meat (noting that most studies did not differentiate between unprocessed and processed red meat) and all-cause mortality, cardiovascular mortality, fatal heart attacks, breast cancer mortality or total cancer mortality. The certainty of the evidence was reported as low or very low in all cases.
It is so important to reiterate that there are no RCTs that have changed red meat alone, not least because it is impossible to change red meat alone. The 1 trial of the 12 that had the most minimal intervention gave participants mushrooms 3x/week or lean beef 3x/week. This would change the intake of all three macronutrients (carbs, fat and protein). This would change the intake of all three fats (saturated, monounsaturated and polyunsaturated). This would change the intake of all micronutrients (vitamins and minerals). This would change the intake of calories. If any effects were found – what made the difference?
Laudable as it may be to try to examine dietary trials for red meat, there are none and there can be none. The most robust conclusion of Paper 2 is that the evidence is very poor.
Papers 3, 4 and 5 (Ref 8)
Papers 3, 4 and 5 were systematic reviews and meta-analyses of cohort studies (also called observational studies or population studies. These are the ones that follow a large number of people for many years to establish associations, not causation). Paper 3 looked at whether a reduction in red and processed meat intake had any impact on cancer mortality and incidence. Paper 4 looked at red and processed meat consumption and all-cause mortality and cardiometabolic outcomes. Paper 5 looked at patterns of red and processed meat consumption and cardiometabolic and cancer outcomes.
In all three papers, there were numerous studies found during the systematic review. The tens of studies included millions of people, followed for up to 34 years. There is no question that the data available are vast. All three papers concluded that any associations observed were very small and the certainty of evidence was low or very low.
– Paper 3 concluded: “The possible absolute effects of red and processed meat consumption on cancer mortality and incidence are very small, and the certainty of evidence is low to very low.”
– Paper 4 concluded: “The magnitude of association between red and processed meat consumption and all-cause mortality and adverse cardiometabolic outcomes is very small, and the evidence is of low certainty.”
– Paper 5 concluded: “Low- or very-low-certainty evidence suggests that dietary patterns with less red and processed meat intake may result in very small reductions in adverse cardiometabolic and cancer outcomes.”
These three papers were summarised succinctly in Paper 1 in Table 1:
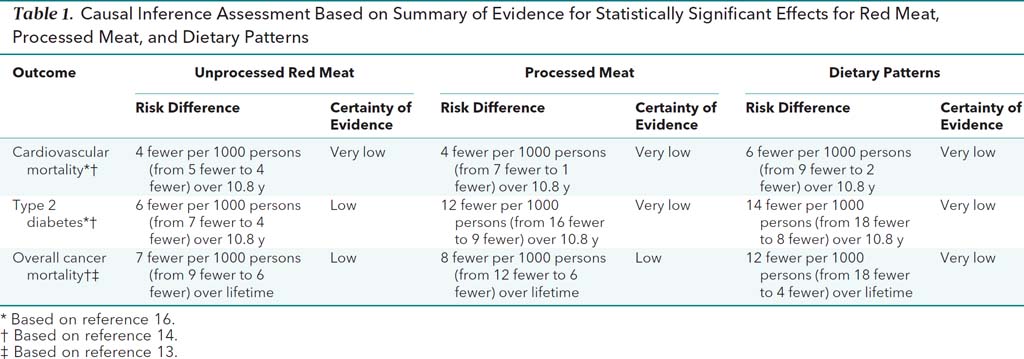
This is a tabular summary of the overall conclusion from the three papers on observational studies: any associations observed were very small and the certainty of evidence was low or very low. (Reference 13 in the table notes is Paper 3 in this note; Reference 16 is Paper 4; Reference 14 is Paper 5).
Paper 6 (Ref 9)
Paper 6 was novel and interesting. This paper looked at studies that tried to evaluate health-related values and preferences regarding meat consumption. If you remember from above, the review determined that willingness to change unprocessed red or processed meat consumption was “critically important” for developing recommendations. There is no point developing dietary guidelines if they are certain or likely to be ignored. I have not seen the ‘propensity to change’ examined before and it is relevant and interesting.
Paper 6 found 54 studies that reviewed attitudes towards meat consumption. 38 addressed reasons for meat consumption: 13 reported that omnivores enjoy eating meat; 18 reported that omnivores consider meat essential as part of a healthy diet and 7 reported that they believe they lack the skills to prepare satisfactory meals without meat (I would not have thought of that). The conclusion of the attitude review was that omnivores are generally unwilling to change their meat consumption.
Some of the subset analysis was interesting. A number of studies found that men were more attached to meat consumption than women. Studies in the elderly reported inconsistent findings. Elderly omnivores were concerned about health aspects of their food – for some that was likely to make them think that they should eat less meat while others thought that meat was necessary to maintain health. Where the studies reported reasons for being vegetarian/low consumers of meat, health was the primary reason given for avoiding meat. This should be seen as encouraging to farmers, as health and meat facts are in their favour and facts are easier to counter than emotional animal reasons for avoiding meat. Many omnivores thought that they had reduced meat intake already and weren’t prepared to reduce it more. Some omnivores were not concerned about any consequences of meat consumption, as they considered these to be trivial relative to other behaviours (e.g., smoking). Many participants were mistrustful of information given out by health authorities.
The reaction to the papers
The reaction was swift and unsurprising. Proponents of the current guidelines were quick to attack the papers and the authors. The first thing that I noticed in the first media article I read was that the word “controversial” appeared in the first sentence. Normally nutritional epidemiological studies are reported as the press release sets out and then the final paragraph takes a quotation from an alternative viewpoint for balance. E.g. under a headline “one glass of juice a day raises risk of cancer”, 95% of the article will cover the press release and then there will be a comment from (for example) the food and drink federation rebutting the latest research. The media articles covering this story devoted more column inches to the rebuttal than they did the findings.
Medscape ran a critical article on the publication date (Ref 10). The (plant-based) True Health Initiative issued a press release rebuttal in parallel with the publication of the articles in the Annals of Internal Medicine (Ref 11). The press release adopted the relative risk position, which was criticised by Paper 1, by presenting a 4 in 1,000 absolute difference as “a 10% reduction in cardiovascular disease mortality.” I didn’t know whether to be annoyed or amused that those who live by nutritional epidemiology are not prepared for it to be used against them.
The True Health Initiative also published a letter demanding that the articles be retracted (Ref 12). Their grounds for retraction showed that they had not read the papers. They argued that PREDIMED and the Diabetes Prevention Programme should have been included. Paper 1 was clear that primary outcomes included mortality and neither of these studies had mortality outcomes. They complained that “qualifying cohort studies” were excluded but listed none. They argued that the fact that the authors reported that the evidence was of “very low certainty” was not a rational basis to recommend – quite the opposite.
An encouraging editorial in the Annals of Internal Medicine makes me think that demands for retraction will be, rightly, rejected (Ref 13). The editorial pointed out “Over and over again, they [the authors] stressed that even if the results were statistically significant, their certainty was low and the absolute differences seen were small and potentially confounded.” The editorial also stated “This is sure to be controversial, but it is based on the most comprehensive review of the evidence to date. Because that review is inclusive, those who seek to dispute it will be hard pressed to find appropriate evidence with which to build an argument.”
A (essentially, if not entirely) non-conflicted panel published four systematic reviews of all the evidence available (which was vast for observational studies, if not RCTs) and concluded that any associations observed were very small and the certainty of evidence was low or very low. They cautioned that observational studies cannot establish causation; they don’t report absolute differences; and they are at high risk of confounding. My conclusion from this would have been to dismiss existing guidelines and advise that they be ignored. The panel’s recommendations to continue current consumption were cautious in this context, not controversial.
References
Ref 1: https://www.pcrm.org/news/news-releases/physicians-group-files-federal-petition-against-annals-internal-medicine-over
Ref 2: https://www.nytimes.com/2019/09/30/health/red-meat-heart-cancer.html?action=click&module=Top%20Stories&pgtype=Homepage
Ref 3: https://www.dailymail.co.uk/health/article-7520483/You-DONT-need-cut-red-meat-scientists-claim-huge-controversial-study.html
Ref 4: https://www.nytimes.com/2019/10/04/well/eat/scientist-who-discredited-meat-guidelines-didnt-report-past-food-industry-ties.html
Ref 5: What is GRADE? https://bestpractice.bmj.com/info/toolkit/learn-ebm/what-is-grade/
Ref 6: Paper 1: Unprocessed Red Meat and Processed Meat Consumption: Dietary Guideline Recommendations. (https://annals.org/aim/fullarticle/2752328/unprocessed-red-meat-processed-meat-consumption-dietary-guideline-recommendations-from)
Ref 7: Paper 2 (Ref 15 in Paper 1): Effect of Lower Versus Higher Red Meat Intake on Cardiometabolic and Cancer Outcomes. A Systematic Review of Randomized Trials. (https://annals.org/aim/fullarticle/2752326/effect-lower-versus-higher-red-meat-intake-cardiometabolic-cancer-outcomes)
Ref 8: Paper 3 (Ref 13 in Paper 1): Reduction of Red and Processed Meat Intake and Cancer Mortality and Incidence. A Systematic Review and Meta-analysis of Cohort Studies. (https://annals.org/aim/fullarticle/2752321/reduction-red-processed-meat-intake-cancer-mortality-incidence-systematic-review)
Paper 4 (Ref 16 in Paper 1): Red and Processed Meat Consumption and Risk for All-Cause Mortality and Cardiometabolic Outcomes. A Systematic Review and Meta-analysis of Cohort Studies. (https://annals.org/aim/fullarticle/2752320/red-processed-meat-consumption-risk-all-cause-mortality-cardiometabolic-outcomes)
Paper 5 (Ref 14 in Paper 1): Patterns of Red and Processed Meat Consumption and Risk for Cardiometabolic and Cancer Outcomes. A Systematic Review and Meta-analysis of Cohort Studies. (https://annals.org/aim/fullarticle/2752327/patterns-red-processed-meat-consumption-risk-cardiometabolic-cancer-outcomes-systematic).
Ref 9: Paper 6 (Ref 17 in Paper 1): Health-Related Values and Preferences Regarding Meat Consumption. A Mixed-Methods Systematic Review. (https://annals.org/aim/fullarticle/2752323/health-related-values-preferences-regarding-meat-consumption-mixed-methods-systematic)
Ref 10: https://www.medscape.com/viewarticle/919221
Ref 11: https://www.truehealthinitiative.org/wp-content/uploads/2019/09/THI-Annals-Meat-Paper-Press-Release.pdf
Ref 12: https://www.truehealthinitiative.org/wp-content/uploads/2019/09/Annals-letter-9-30-19.pdf
Ref 13: https://annals.org/aim/fullarticle/2752329/meat-consumption-health-food-thought






We ate meat for millennia then suddenly it started to make us ill, just as we were eating less of it. Non sequitor.
I suspect a big confounder is the difference between grass-fed meat eaten with vegetables (or not) and grain-fed meat stuffed with hormones and antibiotics, fried in Omega 6 oil and eaten with the bun and the fries and the Big Gulp.
Even then the results are not exactly overwhelming, unless of course you are a Seventh Day Adventist.
I would be surprised that there is a significant difference between any type of meat consumption, grass or grain fed–at least in my home country of America, of which 80 percent of cows are on grassland and their mother’s teat at any one time. Eat nutritionally poor foods (processed carbs) and gain nutritionally poor health.
My daughter, who is doing a psychology phD, sent me a link to Dr. Rangan Chatterjee’s podcast where he interviews Felice Jacka a week ago. Felice studies the effect of diet on mood and was talking about her work. My daughter is looking at the effect of mood on treatment as part of her phD. Interestingly in 2012 Felice published a paper entitled ‘Red Meat Consumption and Mood and Anxiety Disorders’ (https://www.researchgate.net/journal/1423-0348_Psychotherapy_and_Psychosomatics). I can’t access the paper but she says in the podcast that they found a U shaped relationship with too little red meat being bad as well as too much. However she commented that the current dietary recommendations for red meat are too low! In her most recent studies she has used a “Mediterranean diet’ as the healthy diet however her definition includes 3 palm sized portions of red meat per week. Interesting!
Hi Cora
Many thanks for sharing that and all the best for your daughter’s PhD – what a great topic.
Best wishes – Zoe
Happy to see hard work paying off, Zoe.
I’m not sure how many people have got as far as the “Supplemental Content” linked to from the end of the main report. A 22-page PDF. LOTS of extra detail.
As you identify, the GRADE (Grading of Recommendations Assessment, Development and Evaluation) system has been around for more than 10 years. (Apparently work started on it about 2000). This latest set of reports and guidelines shouldn’t have come as a surprise!
Perhaps this should act as a warning-shot across the bows of poor-quality research in future? But given the way the Bradford Hill Criteria also get ignored, that may be a forlorn hope!
I’m glad I’ve now been introduced to GRADE:
https://en.wikipedia.org/wiki/The_Grading_of_Recommendations_Assessment,_Development_and_Evaluation_(GRADE)_approach
Hi Barry
As Nina Teicholz shared in a private twitter chat: “Their claim that GRADE is ill-equipped for nutrition is contradicted by multiple reviews of nutrition previously using GRADE by Nutrirecs, same group that did this one. Search Johnston B to find them all. Also, National Academies’ specifically recommended GRADE for US Dietary guidelines.”
Best wishes – Zoe
Yay! Thanks again Zoe. Maybe the pendulum has started to swing back.