A story about weight loss
There have been stories in the media recently about well known people who have been taking a diabetes drug for weight loss. Celebrities include Jeremy Clarkson, Elon Musk, Chelsea Handler, and Remi Barder (Ref 1). The drug is called Semaglutide. It is sold under the brand names Ozempic, Wegovy and Rybelsus. Semaglutide is a prescription drug. It is injected into the stomach weekly.
Semaglutide belongs to the class of drug called “incretin mimetics.” They are used for type 2 diabetes (T2D) as they reduce blood glucose levels. The drugs are called “incretin mimetics” because these drugs mimic the effects of incretins. Incretins are hormones produced and released into the blood by the intestine in response to food. The incretin of key relevance with semaglutide is GLP-1 (Glucagon-Like-Peptide-1). GLP-1 increases the release of insulin from the pancreas, slows absorption of glucose from the gut and reduces the amount of glucose being produced by the liver. All three actions are intended to reduce levels of glucose in the blood stream – hence their use for T2D.
Semaglutide was developed by Novo Nordisk in 2012. The drug was originally intended for T2D. It was approved by the FDA for weight loss in June 2021 (Ref 2).
The more scientific articles about the ‘diet craze’ reference the academic study underpinning the drug (Ref 3). The major trial of Semaglutide was published in the New England Medical Journal in February 2021 (Ref 4). I covered it in a note shortly after that publication (Ref 5).
It was a high quality trial – a double-blinded, randomised controlled trial. That means that neither the participant nor the researchers knew who was in each group. That’s the theory. The reality was that the side effects were so pronounced (and the loss of appetite from the drug) that people probably knew which group they were in. The trial was large (1,961 people) and long (68 weeks) and multi-site (129 sites in 16 countries). Novo Nordisk sponsored the trial, designed the trial and oversaw its conduct.
The average BMI was 38 at the start of the trial. The participants were randomly assigned in a 2:1 ratio to the semaglutide injection (2.4mg once a week) or a placebo injection. Both groups also adopted lifestyle changes (counselling sessions every 4 weeks to help participants adhere to a 500 calorie deficit daily and 150 minutes of physical activity per week).
The results were impressive. I reported in my 2021 Monday note that “they were the best I have seen in any drug vs placebo weight loss trial.” I added “they were almost unbelievable.” The enthusiasm for the drug among celebrities suggests that the results might be believable – even though the trial had company conflicts.
The drug does seem to decrease appetite. Clarkson quipped “You can look at a Sunday roast, with gravy and beef and perfect Yorkshire puddings, and you think: ‘I’ll just have a stick of celery instead‘” (Ref 6). In the same article, Chelsea Handler, who stopped taking the drug, was quoted as saying “”But I like having an appetite. It made me nauseous, and I don’t like to be nauseous.”
This brings us to the observations that I made about side effects when I first looked at the NEMJ study. The adverse events reported in the drug group were primarily gastrointestinal: 44% reported nausea; 32% diarrhoea and 25% reported vomiting. Overall, 74% reported gastrointestinal disorders. These numbers were all significantly higher than those reported in the placebo group. Perhaps semaglutide reduced appetite because eating became so traumatic that it wasn’t worth the effort. Diarrhoea and vomiting would reduce absorption of food and this could have impacted weight loss. (It would also have impaired nutrient absorption). Twice as many people in the drug group withdrew from the trial (compared to the placebo group). Nearly 12 times as many people withdrew from the drug group for gastrointestinal reasons as did in the placebo group.
The patient leaflet cautions that serious outcomes include pancreatitis; hypoglycemia; retinopathy (diabetic eye disease), as well as all the gastrointestinal effects reported in the trial (Ref 7). The retinopathy and eye problems are reported to be common serious side effects (affecting up to 1 in 10 people). Other common side effects include gas, bloating, gallstones, reflux, heartburn and hair loss. Acute pancreatitis is reported as “may affect 1 in 100 people.” Nausea, vomiting, diarrhoea, constipation, stomach pain and feeling weak or tired are reported as very common (may affect more than 1 in 10 people).
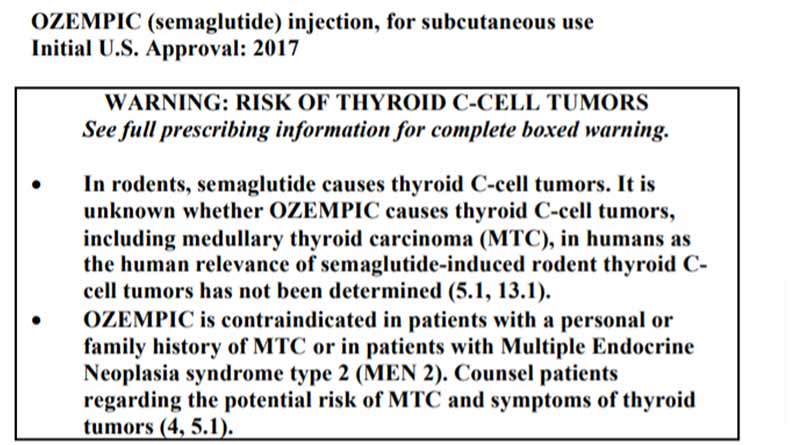
The patient leaflet doesn’t mention the most serious issue. This is prominently featured in the FDA approval document (Ref 8). The header of page one of the approval document has this prominent warning about thyroid cancer.
There is another issue with semaglutide, which celebrities taking it may not yet have realised. The drug needs to be taken on an ongoing basis. The weight loss is reversed if the drug is stopped.
A double-blinded, randomised controlled trial studied the effect of switching people from semaglutide to placebo after 20 weeks of all participants taking semaglutide (Ref 9). Those who continued to take semaglutide continued to lose weight. They had an average (mean) body weight loss from week 20 to week 68 of 7.9%. Those who were switched to a placebo gained 6.9% body weight on average.
The lead author for this study reported receiving speaker fees, consulting fees, and honoraria from Novo Nordisk and being a shareholder in Novo Nordisk. Hence, it could be argued that she had an incentive to find that the drug should be continued. The differences of 7.9% loss vs 6.9% gain are so large that I suspect author conflicts are irrelevant. It is fair to conclude that stopping the drug will lead to weight being regained.
One celebrity who does appear to have worked this out is Remi Barder. She found that her binge eating became worse after she stopped taking the weekly injection. Barder reported gaining double the weight back when she stopped.
This brings us to the lessons from our second story. Whatever you are doing to lose/maintain weight must be sustainable. If it isn’t, you may as well stop now, because you’ll regain if you do stop. Dr Michael Mosley’s latest book, The Fast 800 Keto, is based on 800 calories a day, with carbohydrates under 50g per day and protein above 50g (Ref 10). Unless you can keep this up, you are highly likely to regain when you stop (Ref 11). If, for another example, you are trying to live on one meal a day, unless you can keep this up, you are highly likely to regain when you stop.
People are so desperate to lose weight that they do unwise and often dangerous things. Semaglutide strikes me as more unwise and more dangerous than most other options. An up to 1 in 10 chance of retinopathy and eye problems… An approximate 1 in 100 chance of acute pancreatitis… An unknown risk of thyroid cancer… And a virtual guarantee of weight regain – and possibly more – unless weekly stomach injections are continued for life. Elon Musk is one of the brightest people in the world and he’s doing one of the dumbest things to lose weight (Ref 12). That just shows how powerful the desire to be slim is.
p.s. a recent (rodent) study found that this drug increases the risk of intestinal blockage, which can be fatal.
References
Ref 1: https://www.newsweek.com/celebrities-hollywood-weight-loss-diabetes-drug-ozempic-1774677
Ref 2: https://www.fda.gov/news-events/press-announcements/fda-approves-new-drug-treatment-chronic-weight-management-first-2014
Ref3: https://www.scientificamerican.com/article/new-antiobesity-drugs-help-people-shed-dozens-of-pounds-but-they-must-be-taken-for-a-lifetime/
Ref 4: Wilding et al. Once-Weekly Semaglutide in Adults with Overweight or Obesity. NEMJ. February 2021. https://www.nejm.org/doi/pdf/10.1056/NEJMoa2032183
Ref 5: https://www.zoeharcombe.com/2021/03/semaglutide-weight-loss/
Ref 6: https://www.newsweek.com/celebrities-hollywood-weight-loss-diabetes-drug-ozempic-1774677
Ref 7: https://www.medicines.org.uk/emc/files/pil.13803.pdf
Ref 8: https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/209637s003lbl.pdf
Ref 9: Rubino et al. Effect of Continued Weekly Subcutaneous Semaglutide vs Placebo on Weight Loss Maintenance in Adults With Overweight or Obesity: The STEP 4 Randomized Clinical Trial. JAMA. April 2021. https://pubmed.ncbi.nlm.nih.gov/33755728/
Ref 10: https://thefast800.com/how-to-do-the-fast-800-keto/
Ref 11: Franz et al. Weight-loss outcomes: a systematic review and meta-analysis of weight-loss clinical trials with a minimum 1-year follow-up. J Am Diet Assoc. 2007. https://pubmed.ncbi.nlm.nih.gov/17904936/
Ref 12: https://twitter.com/elonmusk/status/1576367983051489281
Fasting + Ozempic/Wegovy + no tasty food near me
— Elon Musk (@elonmusk) November 16, 2022



Thanks for the prompt reply Dr. Zoe!
Unsurprisingly you’re very well informed about salt!
I think processed foods are so toxic that consumers will still have excess toxicity even with adequate salt and blood volume. So, lack of salt is just one of many factors that could lead to excess burden on the body’s detox mechanisms.
I think you’re aware of research linking low salt to health problems like obesity.
Here’s some research about fat as depository for toxins:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6101675/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3569705/
Additionally, eating lots of salty processed foods/snacks might also be due to avoidance of salt during proper meals, and chronic stress also leads to increased salt craving (which helps):
“stress, which causes high blood pressure, can also cause increased salt intake.” In fact, Henry’s research even ends by saying “the evidence today argues that the most important factor in the etiology of essential hypertension is not salt but psychosocial stimulation .”
https://aletenutrition.com/blogs/saltstick-blog/stress-and-salt-intake
P.s. I suppose the war on salt also benefits the pharma industry, with all the health problems related to insufficient salt/blood-volume and consequently increased chronic stress/anxiety (stress/anxiety is induced by hormones released for vasoconstriction in response to suboptimal blood volume).
You only have to think about what a poor experience it is to eat modern bread to realise that people are not eating it for pleasure. Gliadorphin or gliadin derived peptide are addictive. Blaming the individual or taking pills are really completely irrelevant pending real engagement with the war that the food and health industries are waging on our bodies and minds.
Hi Paul
Too true! Modern bread also rolls up into a tiny ball and ends up looking like play dough!
Best wishes – Zoe
When I was a working GP, we tended to favour GLP 1 agonists and Metformin for Type 2 diabetes, because they reduced appetite and thus made people eat less. The other drug group, Flozins, encouraged loss of sugar in the urine, thus reducing blood sugar levels. All of these drugs were preferable to anything that raised blood insulin levels, basically sulphonylureas, which increased the patients own pancreatic insulin secretion, or insulin injections.
Why preferable? Because the increased insulin, itself a risk factor for vascular disease and hypertension, would get the blood sugar down by helping it to enter cells where it would be turned into fat, driving obesity. ‘Tidying away out of sight’ rather than not allowing it in in the first place, or getting it out of the body, as flozins do.
Far fewer of these drugs would be necessary if the patients were eating the proper diet, ie one low in sugar and starch, but that is the very opposite of what the UK dietitians were promoting, namely one low in saturated fats, with about 60% carbohydrate. This diet not only fuels hunger, but it is feeding the diabetics the very thing that they don’t need!
For about the last 5 years of my time as a GP I pushed the low carb diet approach, with some success, but the whole drug-heavy unhealthy-diet driven approach to diabetes is a big battleship to turn around, after 45 years going in the wrong direction, so anything that puts people off the drugs and on to the right diet can only be a good thing in the long run.
Hi Meddyg
That’s really interesting from the coal face – thank you for sharing.
I’m totally with you on the eatbadly plate – as you know! Not only does it fuel hunger, the high carb diet is addictive. I know this is vehemently denied, but I’ve seen carb addiction in virtually everyone with a weight problem. People want to be slim more than anything and yet they find themselves eating biscuits. Why would that be?!
Best wishes – Zoe
Weight loss is the result of a healthy lifestyle not the goal. All drugs are poison and best avoided especially if you are not sick!
Bang on! Super succinct :-)
Best wishes – Zoe
Currently, I’m most convinced by the theory that excess body fat build-up is due to excess toxicity/waste that the body can’t process fast enough, thus gets stored with/as body fat.
A dominant public health advice is for people to minimise/fear salt intake, which leads to decreased blood/lymph/etc. fluid volumes, thus excess stress on the circulatory-related systems and cascading effects on entire body, leading to excess toxicity/waste in the body.
Increased sugar-craving tends to happen with lack of salt and unhealthy lifestyles, perhaps as a response to enable easier dumping of excess toxicity/waste into/as fat.
Exercise, especially of the legs, could help increase muscle tone, to better circulate blood/lymph, but could be negated if the increased salt loss from perspiration isn’t balanced by increased salt intake.
Could you help explore these, Dr. Zoe? Would be great if you could add credibility to such theories if they are true.
Your semaglutide article is great for sharing with would-be victims, thank you!
Hi Joseph
I’ve not heard of that theory before.
I don’t think that salt should be demonised (https://www.zoeharcombe.com/2013/03/salt-awareness-week-10-things-to-be-aware-of/) but people who eat processed food tend to eat more salt so I’m struggling with the basic logic of the hypothesis. If someone has written a paper on it, please share :-)
Best wishes – Zoe
Hi Dr. Zoe,
Here’s a paper about hypovolemia-induced obesity/diabetes.
https://www.metabolismjournal.com/article/S0026-0495(09)00267-4/fulltext
Low salt intake happens to cause hypovolemia to varying extents.
For those who get enough salt/blood -volume, various toxins would be the causes of obesity:
https://www.theguardian.com/environment/2022/may/19/environmental-toxins-are-worsening-obesity-pandemic-say-scientists
Hi Joseph
Many thanks for these. I keep a running list for possible topics for my Monday note. I’ve put this on there. Just a caution – I receive many more suggestions every week than the one that I can do, so many don’t get done. This might make it or might not! I never know until I start the next one.
Best wishes – Zoe