Lowering LDL
On 10th November, 2018, the American Heart Association (AHA) published new cholesterol guidelines (Ref 1). The document is on open view; it’s 120 pages long. There is a list on page 5 called the “Top 10 Take-Home Messages to Reduce Risk of Atherosclerotic Cardiovascular Disease Through Cholesterol Management.” That says it all really.
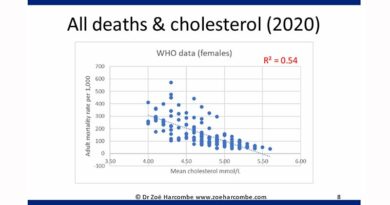
The 10 take-home messages are essentially about ‘statin therapy’ (which is a term that I loathe, as therapy means to relieve or heal and this terminology is intended to masquerade the fact that statins can cause harm. I will only use it forthwith when I am making direct quotations from the guidelines). The first point to make is that the 10 messages are entirely about Low Density Lipoprotein-cholesterol and not total cholesterol. This is interesting. Total cholesterol is no longer the bad guy – that spot is reserved for LDL-cholesterol. But how can that be when cholesterol is cholesterol?! We shall see…
The new guidelines
The guidelines for people with atherosclerotic cardiovascular disease (ASCVD) are to “reduce low-density lipoprotein cholesterol (LDL-C) with high intensity statin therapy or maximally tolerated statin therapy. The more LDL-C is reduced on statin therapy, the greater will be subsequent risk reduction. Use a maximally tolerated statin to lower LDL-C levels by ≥50%.”
The guidelines for people with very high-risk ASCVD are to consider adding nonstatins to statins. The guidelines recommend that the drug Ezetimibe should be used alongside ”maximally tolerated statin therapy.” When LDL-C remains ≥70 mg/dL (≥1.8 mmol/L), even with “maximally tolerated statin and ezetimibe therapy”, the guidelines say that “adding a PCSK9 inhibitor is reasonable, although the long-term safety (>3 years) is uncertain and cost effectiveness is low at mid-2018 list prices.”
The 10 points continue in this way – each point addressing a different group of people defined by age, ASCVD risk, having diabetes or not and LDL-C levels. Patients with “severe primary hypercholesterolemia” are defined as having an LDL-C level ≥190 mg/dL [≥4.9 mmol/L], which is the lowest bar for hypercholesterolemia that I have seen.
The guidelines are ruthless: intensive statin use; administer statins at the highest level that can be tolerated by the patient; add in more drugs if statins alone can’t dramatically curtail LDL-C – even where safety beyond 3 years is unknown and doing this is not cost effective (as is the case with PCSK9s).
Point 10 is about adherence – the American Heart Association (AHA) clearly thinks that there is no point setting these brutal guidelines unless people follow them. Lipid measurements should be repeated 4 to 12 weeks after starting statins, or changing the dose, and then repeated every 3-12 months as needed (to check compliance).
The AHA belief that “LDL-C is a primary cause of atherosclerosis” is absolute and unequivocal. Statins lower LDL-C and therefore statins should be administered to the “maximally tolerated” level. It all seems very clear and simple and the vast majority of people in the so-called developed world are convinced that this is the truth.
At this stage it is pertinent to point out that the sponsors of the AHA are the who’s who of the statin pharmaceutical industry (Ref 2). It is also pertinent to point out that one statin alone, Lipitor, has been worth $125 billion to Pfizer since 1997 (Ref 3). This statin is the most lucrative drug in the world. It is not the only statin. For me, this is the only fact that can explain the obsession with lowering LDL-C, because when you start with the facts about cholesterol, this obsession does not make sense…
The rest of this article is available to site subscribers, who get access to all articles plus a weekly newsletter.
To continue reading, please login below or sign up for a subscription. Thank you.