The Seven Countries Study – Part 2
Response to The True Health Initiative White Paper
On 1st August 2017, a white paper was published called “Ancel Keys and the Seven Countries Study: An Evidence-based Response to Revisionist Histories.” It was commissioned by an organisation called The True Health Initiative and it was written by Katherine Pett and three members of the council of The True Health Initiative: Joel Kahn; Walter Willett; and David Katz.
The white paper was focused on “four primary allegations”, which it claimed had been proposed to discredit Keys and which it claimed were wrong. Part 1 of the review of The True Health Initiative paper found that only one part of one of four allegations – the confusion between the Mount Sinai presentation six countries graph and the seven countries study – is commonly made in error. The rest was much ado about nothing, as Shakespeare would say.
In this second part, I will present the criticisms of the Seven Countries Study (SCS) that the white paper should have made. There are many limitations of the Seven Countries Study. I will cover the six most damning. The first issue alone renders the SCS redundant. (If you would rather watch a video to tell this story, here’s one from February 2017 on this very topic).
1) The SCS is an epidemiological study.
The SCS might be of interest if there were not Randomised Controlled Trials (RCTs) and, better still, systematic reviews and meta-analyses of RCTs, examining dietary fat and heart disease. But there are: many of each. At the time the dietary guidelines were introduced (1977 US/1983 UK) there were five RCTs available for the US authorities to consider (Refs 1-5) and a sixth was available to the UK committee (Ref 6).
Individually, none of these RCTs recommended that dietary guidelines should be introduced. On the contrary, only one study made a positive claim for its intervention after five years (Ref 7) and subsequently, this was moderated (Ref 4). Rose et al (Ref 1) warned of possible harm by administering corn oil. The Research Committee concluded “A low-fat diet has no place in the treatment of myocardial infarction” (p504) (Ref 2). The MRC Soya-bean oil intervention found no evidence that MI relapse would be materially affected by unsaturated fat in the diet (Ref 3). The LA Veterans study reported that total longevity was not affected and expressed concern about unknown toxicity of their intervention (Ref 5). Woodhill et al noted that survival was significantly better in the control than the diet group (Ref 6).
Collectively, in meta-analysis, these RCTs found that dietary interventions made no difference to deaths from Coronary Heart Disease (CHD) or deaths from any cause (Ref 8).
If we generously ignore the fact that the dietary fat guidelines had no RCT evidence base at the time they were introduced, but see if they would be justified now with evidence currently available, I found that they would not be (Ref 9). Others have found similarly. A number of meta-analyses of RCTs, examining dietary fat and mortality, have been undertaken by other authors (Refs 10-13). A meta-analysis of prospective cohort studies has been undertaken by other authors, Siri-Tarino et al (2010) (Ref 14). Two additional meta-analyses reviewed both RCTs and prospective cohort studies (Refs 15, 16).
Table 7.1 in this paper (on open view) (Ref 17) summarised the findings from these other meta-analyses of RCTs and/or prospective cohort studies. There were 39 reports of risk ratios from meta-analysis with 95% confidence intervals. Of these, 4 reported significant findings; 35 reported no significant findings. That is important in itself. 35 out of 39 findings from 8 meta-analyses (Refs 8 and 10-16) found nothing statistically significant in an examination of dietary fat RCTs and/or cohort studies.
The four significant findings were:
i) Chowdhury et al found that trans fat intake was positively associated with coronary disease (Ref 16). I’m not surprised. Having examined the evidence between coronary disease and fatty acids – including saturated, monounsaturated, polyunsaturated and trans fats, while also reviewing individual chain length fatty acids, palmitic (C16:0) and margaric (C17:0) – Chowdhury et al’s conclusion was “Current evidence does not clearly support cardiovascular guidelines that encourage high consumption of polyunsaturated fatty acids and low consumption of total saturated fats” (p398) (Ref 16).
ii) Mozaffarian et al reviewed the impact of replacing saturated fat with polyunsaturated fat (Ref 12). This study was criticised by Ravnskov et al (including me) (Ref 18) for excluding two studies that would have moderated this conclusion – the Rose Corn oil trial (Ref 1) and the Sydney Diet Heart Study (Ref 6) – and for including a favourable, but non-randomised, non-controlled, cross-over, trial excluded by robust meta-analyses – the Finnish Mental Hospital Study (Ref 19). Interestingly, the recent American Heart Association ‘Presidential Advisory’ paper (Ref 20), also unfairly excluded the Rose Corn oil trial (Ref 1) and the Sydney Diet Heart Study (Ref 6) and also unfairly included the Finnish Mental Hospital Study (Ref 19) and funnily enough reached the same biased conclusion as Mozaffarian et al.
iii) & iv) The other two significant findings were related to cardiovascular disease (CVD) events and not mortality (Refs 11, 13). In 2011, including RCTs with a minimum of 6 months duration, Hooper et al (Cochrane review) found 1 significant result and 11 non-significant results. The one significant result was that, when all RCTs were examined together, the risk ratio (RR) for CVD events from meta-analysis was 0.86 (95% CI 0.77 to 0.96). In 2015, including RCTs with a minimum of 24 months duration, Hooper et al found one significant result and seven non-significant results. The one significant result was that, when a reduction in saturated fat was examined, the risk ratio (RR) for CVD events from meta-analysis was 0.83 (95% CI 0.72 to 0.96).
As a result of this 2015 review (an update of the 2011 review), Hooper et al suggested that there may be a small reduction in cardiovascular risk with reduction of saturated fat intake (Ref 13). It was further suggested that replacing the energy from saturated fat with polyunsaturated fat “appears to be a useful strategy, and replacement with carbohydrate appears less useful” (p2) (Ref 13) and replacement with monounsaturated fat unclear. However, of the 11 interventions contributing to this conclusion, only 1 documented both saturated fat reduction and reported that this was mainly replaced with polyunsaturated fat (Ref 5).
This prompts the question – why would Hooper et al have found even one significant result (among many non-significant results) that other researchers didn’t? The Hooper et al meta-analyses of 2011 and 2015 included four small studies (646 people in total), not included in other meta-analyses, which were primarily studies of: diabetes (Ref 21); skin cancer (Ref 22); hypercholesterolemia (Ref 23); and glucose intolerance (Ref 24), but for which Hooper et al obtained CVD event information from correspondence with authors. This non-published data was also, therefore, not peer reviewed. Some of it required only a cursory examination to establish that it was nutritionally unsound: Houtsmuller described the intervention diet as “carbohydrates 50 cal%, saturated fats 35 cal% and proteins 15 cal%” (Ref 21). As there is no food containing saturated fat without unsaturated fat, this diet cannot exist.
Notwithstanding that Hooper et al reached a conclusion using non peer reviewed, non robust data… Notwithstanding that Hooper et al reported a finding about replacing saturated fat with polyunsaturated fat, when only one study had actually done this… (and did not recommend dietary change)… when Hooper et al subjected their one significant finding (for CVD events) to the required sensitivity analysis, even this one finding ceased to be statistically significant (Table 8, p121) (Ref 13), leaving no genuine significant findings. (I always credit Dr Trudi Deakin for alerting me to this point).
For the final nail in the Hooper et al coffin, the most recent review (2015) (Ref 13) included no study of healthy people of both genders. The one primary, both-sex RCT available was excluded by Hooper et al, for not meeting the 24 month duration criteria (Ref 25). Even if the one claim of a small benefit for CVD events had been robust, this had no “generalisability” and thus could not be applied to people from the general population. i.e. you and me.
It is worth remembering that dietary fat guidelines were introduced with the ambition of reducing deaths from CHD. No meta-analysis of RCTs and/or prospective cohort studies has found any significant difference for dietary fat interventions and all-cause mortality or deaths from CHD, or associations with dietary fat and CHD mortality (Refs 8 and 10-16).
2) The SCS contradicted contemporary epidemiological and RCT evidence.
In Part 1 of the review of The True Heath Initiative white paper, in the “In Addition” section, I quoted an extract from p5 of the white paper: “Ultimately, SCS suggested a link between dietary intake, specifically saturated fat, and heart disease. This conclusion, which corroborated other clinical and epidemiological evidence at the time, generated numerous hypotheses and has since inspired countless clinical trials.”
I said that this was not correct: “The finding between saturated fat intake and heart disease was not replicated by other clinical or epidemiological evidence at the time” (Refs 8, 26). The RCT evidence has been presented above. The six RCTs at the time neither individually, nor collectively, corroborated the SCS finding; quite the opposite.
Turning to epidemiological evidence, the six epidemiological studies of the time were: The Western Electric Study (Ref 27); The Seven Countries Study (Ref 28); a study conducted in London and the South East (Ref 29); The Framingham Heart Study (Ref 30); The Honolulu Heart Program (Ref 31); and The Puerto Rico Heart Health Program (Ref 32). The systematic review of these six epidemiological studies was an original publication from my Ph.D. (Ref 26). The summary table of evidence from the six studies is below:
Table 1 Outcome data from included prospective cohort studies for: study name; participant number and age range; years of follow-up; total fat and saturated fat for CHD-free vs. CHD deaths (Refs 30-32) or CHD-free vs. development of CHD (Refs 27-29); and other significant associations found.
| Study |
Men/Age (*) |
Follow-up yrs |
Total fat & CHD assoc? |
Sat fat & CHD assoc? |
Other Significant associations with CHD |
| Western Electric Study (Ref 27) |
1,989 |
4 |
No |
No |
Smoking/age of death of father/coffee |
| Seven Countries Study (Ref 28) Note 1 |
12,770 |
5 |
No |
Yes |
Previous MI. NO association found with smoking/ activity or weight |
| London bank and bus study (Ref 29) |
337 |
20 |
No |
N/A |
Smoking/Age of participant/Inverse with higher calorie intake |
| Framingham (Refs 30, 33) |
859 |
4 |
No |
No |
Inverse with higher calorie & higher alcohol intake (Note 2) |
| Honolulu (Refs 31, 33) |
7,272 |
6 |
No |
No |
Inverse with higher calorie & higher alcohol intake |
| Puerto Rico (Refs 32, 33) |
8,218 |
6 |
No |
No |
Inverse with higher calorie & rural living |
|
Table notes: N/A = data not available; MI = Myocardial Infarction; CHD = Coronary Heart Disease. |
All six studies, including the SCS, concluded that total fat was not associated with heart disease (Ref 26). The white paper acknowledged this: “Though SCS itself never concluded that total fat intake should be restricted” (p5). (It does make you wonder how the total fat restriction of 30% ever happened). The SCS was alone in finding that saturated fat and coronary heart disease (CHD) were associated. The SCS also asserted that smoking, activity levels/exercise and weight played no part in CHD. Much importance was assigned to a study for its saturated fat findings, which contradicted contemporary evidence about smoking, activity and weight.
3) An inter-country study is fundamentally confounded.
P14 of the white paper tried to position an inter-country study as preferable to a study of the same populations: “Researchers carefully selected populations across a wide variation of dietary patterns, but with low variance of other characteristics to limit confounding.” Good luck with that one! This is a fundamental flaw of the Seven Countries Study; it is not a positive attribute.
The five non-SCS contemporary epidemiological studies listed above all studied the same populations. They studied men with location, climate, political environment, health care access and much more in common. They were looking to assess which dietary and lifestyle differences, within the same population, were associated with CHD.
The SCS was an inter-country comparison rather than a CHD/CHD-free comparison. Men who developed CHD in Japan were compared with men who developed CHD in the US, as opposed to men who developed CHD in Japan being compared with men who did not develop CHD in Japan. The SCS would have us believe that CHD in Japan vs. CHD in the US was down to the percentage of calories derived from saturated fat in the diet. Not geography, not climate, not lifestyle, not community, not connectivity to the land, not being a fisherman vs. being a railroad worker, not national Gross Domestic Product, not politics, not the amount of fish consumed vs. the number of hot dogs consumed…
4) The SCS wasn’t a robust dietary study.
The dietary information available from The Seven Countries Study was not comprehensive. Dietary information was documented in Volume XVII of The Seven Countries Study (Ref 34) and in a non-mainstream Dutch booklet (Den Hartog) (Ref 35). Most of the volumes in Circulation made no mention of dietary fat: total, saturated or any other kind (Refs 36-46). My Ph.D. thesis fully documented the few references to diet/dietary fat in the original Circulation 20 volumes and noted the striking omissions. There was no dietary information in either Circulation or Den Hartog for the USA railroad cohort or the Rome railroad cohort and Japan was not covered by the Den Hartog publication. The three Yugoslavian cohorts of Velika Krsna, Zrenjanin and Belgrade were reported in Volume XII of The Seven Countries Study (Ref 40), but there were no references to diet or dietary fat. The Den Hartog booklet reported percentage of calories from each macronutrient for these three cohorts, but with no food intake detail underpinning this.
To give you an idea of how poor dietary references were when they were made, here is one from Volume VIII in Circulation about the Dutch cohort of Zutphen (which tells us nothing about the Dutch diet): “…the data on the U.S. railroad men are not very precise, but the Americans seemed to be more like the Zutphen men than any other cohort in respect to total fats, kinds of fatty acids, etc” (pI-81) (Ref 47).
The opening volume of the study reported that 7-day dietary surveys were carried out on random samples of the cohorts, except in the United States where dietary data were obtained by 24-hour recall interview of all men at the time of entry examination and among the Rome railroad men, where a sample of employees were queried with the sole purpose of detecting whose diets differed from the norm for the region. For Japan, it was noted that a more carefully controlled survey was carried out at Tanushimaru, but not at the fishing village of Ushibuka (pI-6) (Ref 28). Aside from the US survey, the highest sample taken was 8.1% in Yugoslavia – Zrenjanin – and the lowest sample taken was 2.8% in Italy – Crevalcore. From data available, I calculated the average number of men sampled to be 3.4%. That cannot constitute a robust dietary study.
5) Keys was aware of the impact of war, but the SCS ignored it.
The context of The Seven Countries Study was important, as the men were war survivors. Men aged 40-59 years in 1956 (when the SCS started in preparation) were aged between 23-42 years when World War II started and aged between 29-48 years when World War II ended.
The True Health Initiative white paper made 13 references to war/World War II and Keys also made a number of references to World War II in his publications. Keys was aware of the impact of war on countries studied, Finland especially. Keys excluded Finland from the 1953 Mount Sinai presentation/six countries graph with the explanation: “The omissions are Western Germany and Finland, because of major population shifts and other effects from the war” (p120) (Ref 48). In the 1954 symposium on atherosclerosis, Keys described the impact of war on the four Scandinavian countries (p190) (Ref 49). In a 1952 paper, Keys narrated: “Besides the dubious point of attributing war-time changes in vital statistics to actual changes in atherosclerosis…” (p115-116) (Ref 50).
Despite this knowledge, Keys included Finland (east and west) in the Seven Countries Study. The greatest suffering directly involving any of the 16 cohorts was experienced in east Finland. The Finns fought the Winter War alone against the Soviet Union, the Continuation War with Germany against the Soviet Union and the Lapland War against Germany. Most of Finnish Karelia was lost to the Soviet Union with The Moscow Peace Treaty of 1940. Approximately 400,000 people, virtually the entire population of east Finland, were displaced as a result of World War II. I joked in my 2010 book The Obesity Epidemic, I think I would have had a heart attack after all that! For the years following the war (the years of the Seven Countries Study), east Finland experienced the highest rate of CHD deaths among all 16 cohorts – 3 to 4 times higher than the rates in west Finland, despite similar intakes of total fat and saturated fat. Keys was aware of the impact of war, but didn’t acknowledge it in the Seven Countries Study.
The devastation that World War II inflicted upon east Finland/north Karelia is important to remember because this region is often heralded as an example of how changing dietary fat intake can impact heart disease (Ref 51). The SCS confirmed that CHD mortality was greatest in this cohort. Which explanation do you consider the most plausible (especially given the diet similarity, but immense mortality difference, between east and west Finland)? i) CHD mortality was profoundly impacted by years of war and displacement. CHD mortality reduced thereafter because a) men can’t die twice and b) the next generation did not endure the war. Or ii) north Karelia swapped butter for rapeseed oil based margarine.
6) There were better correlations observable.
As this fabulous web site shows, “spurious correlations” can be found between many different variables ( Yudkin reported “By far the best correlation I have found with trends in coronary mortality is in the number of radio and television licences (fig.24). There is nearly as good a correlation with the number of registered motor-vehicles” (p159) Ref 52).
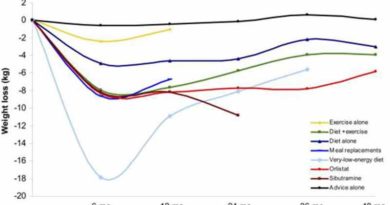
The 25 year follow-up to The Seven Countries Study (Ref 53) calculated Pearson correlation coefficients for mean serum cholesterol levels at baseline and CHD deaths at 5, 10, 15, 20 and 25 years of follow-up. The Pearson correlation coefficient was calculated as 0.72 for baseline cholesterol and CHD deaths at 25 years. I used the data in the 1993 Menotti article to repeat the correlations found with CHD death rates and mean serum cholesterol to understand the data and methodology used. The same methodology was then used to explore alternative correlations. The strongest relationship found was for CHD death rates and the latitude of the country or cohort in The Seven Countries Study. The correlation coefficient for CHD deaths and latitude of the cohort was 0.93. The correlation coefficient for CHD deaths and latitude of the country was 0.96. That is an almost perfect correlation.
The latitude finding offers an alternative explanation for the observed relationship with cholesterol and CHD. Vitamin D is made when sunshine synthesises cholesterol in skin membranes (Ref 54). In cohorts further away from the equator, cholesterol is less able to be turned into vitamin D. Population mean serum cholesterol levels are higher and concomitantly population mean vitamin D levels are lower. Higher CHD could be associated with lower vitamin D, with cholesterol a marker, not a maker, of heart disease and dietary fat having no more to do with anything than television sets (Ref 55).
In conclusion
As an epidemiological study, The Seven Countries Study could only suggest associations. It has been afforded inappropriate regard for its saturated fat finding, while it was simultaneously wrong about exercise, weight and smoking. As an epidemiological study it is superseded by RCT evidence and systematic reviews/meta-analyses (of RCTs and/or epidemiological studies). The saturated fat finding from the Seven Countries study was not supported by six RCTs and five other epidemiological studies of the time. (That total fat was not associated with CHD was supported, but remains little known). 8 systematic reviews and meta-analyses of dietary fat and coronary mortality have reported nothing of significance in 35 out of 39 findings. The one finding that withstands scrutiny was that trans fat intake is positively associated with coronary disease (Ref 16). The hierarchy of evidence alone renders the SCS redundant. The SCS had many other flaws, which I have covered for the record, but the primary, irrefutable charge is that, 50 years on, there is more and better evidence available and it doesn’t support the SCS.
In Part 1 of my response to The True Health Initiative white paper, I pointed out that the primary sources of saturated fat are junk food (pizza, desserts/cakes/pastries, candy/confectionery, potato chips, biscuits, pasta/bread, tortillas, burritos, tacos, hot dogs and other processed foods). I had thus proposed a way forward in this paper (Ref 17) that real food proponents should unite in our opposition to processed food, but stop demonising saturated fat (where found naturally in foods of animal, or plant, origin) in the name of processed food.
Since writing that, something occurred to me. Andy and I had the joy and privilege of Gary and Belinda Fettke staying with us in July – just before Gary presented at the CrossFit games on 2nd August – and they shared some discoveries that they have made. The Fettkes have uncovered an extraordinary web of ‘medical evangelism’ tracing back to Seventh Day Adventists and their beliefs, the earliest cereal companies and dietetic associations formed 100 years ago. Today, the ‘medical evangelism’ ranges from an Australian processed food company set up by Seventh Day Adventists 120 years ago (and thus paying no tax, as a religious organisation), to the global web of “lifestyle medicine” organisations, of which The True Health Initiative is an integral part.
As I said in Part 1, I share the “minimally processed food” beliefs of this ‘medical evangelism’, but the nutritional evidence does not allow me to share their plant-based-diet ideology. If the priority of this ‘medical evangelism’ were the “minimally processed” part, my way forward could and would be accepted. We could unite in our opposition to processed food and celebrate our common ground. However, the fact that the saturated fat misconception continues to be made tells me that the primary agenda is pushing plant-based food and not the “minimally processed” part. For as long as the agenda is pushing plant-based food, then saturated fat will continue to be conveniently and wrongly positioned as animal fat and conveniently and wrongly blamed for poor diet, when the real factor in a bad diet is junk food.
The True Health white paper and the research undertaken by the Fettkes has convinced me that ‘medical evangelism’ is synonymous with a plant-based-diet agenda. I invite The True Health Initiative and other lifestyle-medicine/plant-based evangelists to join omnivore real foodies in prioritising “minimally processed” and prove me otherwise.
References
1. Rose GA, Thomson WB, Williams RT. Corn Oil in Treatment of Ischaemic Heart Disease. BMJ 1965.
2. Research Committee. Low-fat diet in myocardial infarction: A controlled trial. The Lancet 1965.
3. Medical Research Council. Controlled trial of soya-bean oil in myocardial infarction: Report of a research committee to the Medical Research Council. The Lancet 1968.
4. Leren P. The Oslo Diet-Heart Study. Circulation 1970.
5. Dayton S, Pearce ML, Hashomoto S, Dixon WJ, Tomiyasu U. A Controlled Clinical Trial of a Diet High in Unsaturated Fat in Preventing Complications of Atherosclerosis. Circulation 1969.
6. Woodhill JM, Palmer AJ, Leelarthaepin B, McGilchrist C, Blacket RB. Low fat, low cholesterol diet in secondary prevention of coronary heart disease. Advances in experimental medicine and biology 1978.
7. Leren P. The effect of plasma-cholesterol-lowering diet in male survivors of myocardial infarction. A controlled clinical trial. Bull. N. Y. Acad. Med. 1968.
8. Harcombe Z, Baker JS, Cooper SM, et al. Evidence from randomised controlled trials did not support the introduction of dietary fat guidelines in 1977 and 1983: a systematic review and meta-analysis. Open Heart 2015.
9. Harcombe Z, Baker JS, DiNicolantonio JJ, Grace F, Davies B. Evidence from randomised controlled trials does not support current dietary fat guidelines: a systematic review and meta-analysis. Open Heart 2016.
10. Schwingshackl L, Hoffmann G. Dietary fatty acids in the secondary prevention of coronary heart disease: a systematic review, meta-analysis and meta-regression. BMJ Open 2014.
11. Hooper L, Summerbell CD, Thompson R, et al. Reduced or modified dietary fat for preventing cardiovascular disease. Cochrane database of systematic reviews (Online) 2011.
12. Mozaffarian D, Micha R, Wallace S. Effects on coronary heart disease of increasing polyunsaturated fat in place of saturated fat: a systematic review and meta-analysis of randomized controlled trials. PLoS Med. 2010.
13. Hooper L, Martin N, Abdelhamid A, Davey Smith G. Reduction in saturated fat intake for cardiovascular disease. Cochrane Database of Systematic Reviews 2015.
14. Siri-Tarino PW, Sun Q, Hu FB, Krauss RM. Meta-analysis of prospective cohort studies evaluating the association of saturated fat with cardiovascular disease. The American journal of clinical nutrition 2010.
15. Skeaff CM, Miller J. Dietary fat and coronary heart disease: summary of evidence from prospective cohort and randomised controlled trials. Ann. Nutr. Metab. 2009.
16. Chowdhury R, Warnakula S, Kunutsor S, et al. Association of Dietary, Circulating, and Supplement Fatty Acids With Coronary Risk: A Systematic Review and Meta-analysis. Ann. Intern. Med. 2014.
17. Harcombe Z. Dietary fat guidelines have no evidence base: where next for public health nutritional advice? Br. J. Sports Med. 2016.
18. Ravnskov U, DiNicolantonio JJ, Harcombe Z, Kummerow FA, Okuyama H, Worm N. The Questionable Benefits of Exchanging Saturated Fat With Polyunsaturated Fat. Mayo Clinic proceedings. Mayo Clinic 2014.
19. Turpeinen O, Karvonen MJ, Pekkarinen M, Miettinen M, Elosuo R, Paavilainen E. Dietary prevention of coronary heart disease: the Finnish Mental Hospital Study. Int J Epidemiol 1979.
20. Sacks FM, Lichtenstein AH, Wu JHY, et al. Dietary Fats and Cardiovascular Disease: A Presidential Advisory From the American Heart Association. Circulation 2017.
21. Houtsmuller AJ, Zahn KJ, Henkes HE. Unsaturated fats and progression of diabetic retinopathy. Doc. Ophthalmol. 1979.
22. Black HS, Herd JA, Goldberg LH, et al. Effect of a Low-Fat Diet on the Incidence of Actinic Keratosis. New England Journal of Medicine 1994.
23. Moy TF, Yanek LR, Raqueño JV, et al. Dietary Counseling for High Blood Cholesterol in Families at Risk of Coronary Disease. Prev. Cardiol. 2001.
24. Ley SJ, Metcalf PA, Scragg RK, Swinburn BA. Long-term effects of a reduced fat diet intervention on cardiovascular disease risk factors in individuals with glucose intolerance. Diabetes Res. Clin. Pract. 2004.
25. Frantz ID, Dawson EA, Ashman PL, et al. Test of effect of lipid lowering by diet on cardiovascular risk. The Minnesota Coronary Survey. Arteriosclerosis, Thrombosis, and Vascular Biology 1989.
26. Harcombe Z, Baker JS, Davies B. Evidence from prospective cohort studies did not support the introduction of dietary fat guidelines in 1977 and 1983: a systematic review. Br. J. Sports Med. 2016.
27. Paul O, Lepper MH, Phelan WH, et al. A Longitudinal Study of Coronary Heart Disease. Circulation 1963.
28. Keys A. Coronary heart disease in seven countries I. The study program and objectives. Circulation 1970.
29. Morris JN, Marr JW, Clayton DG. Diet and heart: a postscript. BMJ 1977.
30. Gordon T, Kannel WB. The Framingham Massachusetts Study twenty years later. In: Kessler I, Levin M, eds. The Community as an Epidemiologic Laboratory; A Casebook of Community Studies. Baltimore: Johns Hopkins Press, 1970.
31. Kagan A, Harris BR, Winkelstein W, Jr., et al. Epidemiologic studies of coronary heart disease and stroke in Japanese men living in Japan, Hawaii and California: demographic, physical, dietary and biochemical characteristics. J. Chronic Dis. 1974.
32. Garcia-Palmieri MR, Feliberti M, Costas R, Jr., et al. An epidemiological study on coronary heart disease in Puerto Rico: The Puerto Rico Heart Health Program. Bol. Asoc. Med. P. R. 1969.
33. Gordon T, Kagan A, Garcia-Palmieri M, et al. Diet and its relation to coronary heart disease and death in three populations. Circulation 1981.
34. Keys A. Coronary heart disease in seven countries XVII. The Diet Circulation 1970.
35. den Hartog C, Buzina K, Fidanza F. Dietary studies and epidemiology of heart diseases. The Hague: Stichting tot Wetenschappelijke Voorlichting op Voedingsgebied, 1968.
36. Keys A. Coronary heart disease in seven countries II. Method. Circulation 1970.
37. Keys A. Coronary heart disease in seven countries III. Classification—Codes and Cohorts Circulation 1970.
38. H. L. Taylor, Henry Blackburn, Ancel Keys, R. Willis Parlin, Cesar Vasquez, Puchner T. Coronary heart disease in seven countries IV. Five-Year Follow-up of Employees of Selected U.S. Railroad Companies Circulation 1970.
39. Henry L. Taylor, Alessandro Menotti, Vittorio Puddu, Mario Monti, Keys A. Coronary heart disease in seven countries XI. Five Years of Follow-up of Railroad Men in Italy Circulation 1970.
40. B. S. Djordjević, B. Balog, LJ. Bozinovi, et al. Coronary heart disease in seven countries XII. Three Cohorts of Men Followed Five Years in Serbia Circulation 1970.
41. Keys A. Coronary heart disease in seven countries XIII. Multiple Variables Circulation 1970.
42. Keys A. Coronary heart disease in seven countries XIV. Prevalence. Circulation 1970.
43. Keys A. Coronary heart disease in seven countries XV. Prognosis of Coronary Heart Disease Found at Entry Circulation 1970.
44. Henry Blackburn, H. L. Taylor, Keys A. Coronary heart disease in seven countries XVI. The Electrocardiogram in Prediction of Five-Year Coronary Heart Disease Incidence Among Men Aged Forty through Fifty-Nine Circulation 1970.
45. Keys A. Coronary heart disease in seven countries XVIII. Some Problems Circulation 1970.
46. Keys A. Coronary heart disease in seven countries References. Circulation 1970.
47. Vanbuchem FSP. Coronary heart disease in seven countries VIII. Zutphen, A Town in the Netherlands. Circulation 1970.
48. Keys A. Atherosclerosis: a problem in newer public health. J. Mt. Sinai Hosp. N. Y. 1953.
49. Keys A, Anderson JT. The relationship of the diet to the development of atherosclerosis in man. In: National Research Council DoMS, ed. Symposium on atherosclerosis. Washington: National Academy of Sciences – National Research Council., 1954.
50. Keys A. Human atherosclerosis and the diet. Circulation 1952.
51. Puska P. Fat and heart disease: yes we can make a change–the case of North Karelia (Finland). Ann. Nutr. Metab. 2009.
52. Yudkin J. Diet and coronary thrombosis: Hypothesis and fact. The Lancet 1957.
53. Menotti A, Keys A, Kromhout D, et al. Inter-cohort differences in coronary heart disease mortality in the 25-year follow-up of the seven countries study. European journal of epidemiology 1993.
54. Gillie O. Sunlight robbery: a critique of public health policy on vitamin D in the UK. Molecular nutrition & food research 2010.
55. Scragg R. Seasonality of cardiovascular disease mortality and the possible protective effect of ultra-violet radiation. Int J Epidemiol 1981.





Here are some quotes from one of the papers of The Puerto Rico Heart Health Program. Doesn’t seem very supportive of low-carb diets, does it?
“In the rural area, persons who developed an MI or died from CHD consumed a higher percent of calories from saturated fatty acids.”
“Urban men who developed myocardial infarction or CHD death had significantly lower calorie and carbohydrate intakes i.e. chiefly those derived rice and legumes.”
“Dietary sucrose intake showed no relationship to CHD incidence.”
“an independent inverse relation of carbohydrate intake from legumes to CHD incidence.”
Nice work as always.
When Frank Hu of Unilever, I mean Harvard, subsequently dissociated himself from the results of the Siri-Tarino metastudy, he made himself look rather foolish since there had already been a similar but different metastudy
http://jamanetwork.com/journals/jamainternalmedicine/fullarticle/1108492
which hardly anyone ever seems to have heard of. Andrew Mente appears to be a researcher with integrity. OK only correlations but he thumbs through a lot of them and finds only a few that stand out.
There are a multitude of theories about diet and nutrition; some sound absolutely ludicrous but could have elements of truth.
I am pursuing a hypothesis put forward a decade ago: that the obesity increases matches the sale of microwave ovens.
http://news.bbc.co.uk/1/hi/health/6725775.stm
I read through some of the early dietary studies from the Finland cohorts ( e.g. Roine et al. 1964 https://www.cabdirect.org/cabdirect/abstract/19651400898 ) , and all the Finns were eating a lot of potatoes and bread. Can’t imagine Finland in the winter was an easy place to burn off all those carbs. So any proteins eaten in that context would be more subject to endogenous glycation. Plus a lot of the fat came from drinking milk which was the primary source for vitamin A & D. They didn’t eat a lot of fruit or veg, All the Finnish men supposedly smoked like chimneys.
When you look at later studies from these Finnish cohorts when the men got into their sixties, there are numerous studies on glucose intolerance. Back in the 1980’s, there already was a very large percentage of Finnish men (over 30%) with previously undiagnosed T2DM. So just as likely, or more likely, insulin resistance was a better marker for CHD than LDL serum cholesterol. Potatoes came from Peru, so can’t imagine potatoes were part of evolutionary diets for people in Finland. They probably had more caribou based diets…which includes the lichen from the stomachs of caribou as a veg source.
It seems therefore there were probably several ways to reduce CHD/CVD including not smoking, and reducing all the high glycemic carbs. The various fatty acids in meats (which are more MUFA’s and PUFU’s than SFA’s) probably have little to do with CHD/CVD reduction in Finland when eaten within the context of a healthier diet and lifestyle without the high glycemic carbs and the smoking.
Hi Stefhan
The Den Hartog document has a pretty good break down of the Finnish cohorts. I hope this table vaguely holds structure (the first number in each row is food item and then it has the % of energy for w Finland and then east Finland.) The interesting thing is how similar the diets are – for such a huge difference in CHD mortality – hence why you must factor in war…
As % of energy Finland W Finland E
Number men 30 30
Cereals 32.7% 30.2%
Sugar 10.0% 9.6%
Margarine 2.8% 2.7%
Butter 12.4% 16.7%
Milk 21.3% 23.0%
Meat 7.6% 7.0%
Fish 0.4% 1.7%
Eggs 1.8% 0.7%
Alcohol 0.6% 0.4%
Potatoes 6.1% 5.6%
Other veg 1.5% 1.0%
Fruits 2.1% 0.9%
Other 0.7% 0.5%
TOTAL 100.0% 100.0%
Yeah, War make sense and its something you really can’t deduce from just reading the studies since no context was really given…..Though both Finnish cohorts along with the US cohort were on one side of the CHD/SFA graph while the Greeks and other Med ones were on the other side with less of an association. The Greeks and Italians ate a lot of bread and consume a lot of grains as well, but it’s a lot warmer in Greece and Italy than Finland so men living in these warmer areas could burn off all those excess carbs.
What I find peculiar (well not really considering how much funding Willett at Harvard gets from Unilever) is the infatuation with PUFU’s since none of the Greek or other Mediterranean countries ate much PUFU’s…They all ate mono-unsaturated fats…mainly oleic acids. If any group was eating polyunsaturated fats in excess it would have been the US cohort. But I couldn’t find the specific dietary data for this cohort. These PUFU’s would also most likely have been hydrogenated. WW2 really opened up the door for the switch over from butter to margarine consumption in the US. Here’s a graph: http://www.greeniacs.com/images/stories/article/butter-VS-margarine.jpg The cross over from butter to margarine almost directly coincides with the higher rates of CHD deaths in the 50’s and 60’s…suggesting that transfats were actually to blame.
One other thing, the equating of SFA’s and animal fats is a bit absurd as you point out. Here’s a video https://youtu.be/jWq-o-FNrSQ of my friend’s Mangalitsa pig farm in Northern California. His pigs get over 50% of their diet from forage including acorns. He had the fats tested from his pigs and they were 60% oleic acid. Olive oil is 70% oleic acid. This breed of lard pig was the main source of cooking fat in Central Europe particularly in the Austro-Hungarian Empire. Western Europe including the UK and Spain had (Lincolnshire Curly Coat ) or still have similar breeds of pigs.
Originally in the UK (and probably Europe) margarine was made from milk and beef fat (I got that from Unilever’s website), the stuff based on seed oils and trans fats came here later.
Would be interesting to see if the CVD “epidemic” here correlated with this change.
I’m always impressed by the plant-eaters insistence that low-carb diets are bad for us because “cutting out whole food groups” is dangerous, when they then go on to recommend we cut out another food group: meat.
But there again, logic and religion don’t have a particularly good relationship.
Hi Hugh
Indeed! Meat and fish and eggs and dairy in true plant-based cases! That’s 4 food groups by my reckoning: https://www.zoeharcombe.com/2015/05/food-groups/
Best wishes – Zoe
Hello Zoe,
Have you heard of Dave Feldman?
He managed to reduce his LDL by 30% in 3 days with a diet high in saturated fat.
It would be very interesting to read you on this subject.
Forgive the fault, I use a translation software but I can very well read you.
Thank you
Gilles from Montreal
Hi Gilles
Very much so! We spoke at a conference together in Feb – fascinating work!
Best wishes – Zoe
Will you give us your opinion soon on his researches?
Gilles
Hi Gilles
I’m not sure it warrants an opinion. It’s factual and original. Dave has shown that he can engineer his LDL-cholesterol reading with his dietary fat intake in the preceding 3 days. He has given the plausible mechanism as “LDL’s primary job is to distribute energy from fat.”
Both Dave and I (and many others) still think that cholesterol is not a factor to worry about in heart disease (or anything else), but he has developed a protocol for getting doctors ‘off your back’. My strategy is don’t go near doctors (unless necessary) and then you don’t have to get them off your back!
Best wishes – Zoe
Hehe. You said “pant based”
Sorry.
Wow! Dr. Zoe, you handle studies’ analysis like Picasso handles a brush.
Because she has got M.A in maths
Great wrap-up on the Seven Countries response, Zoe!
And thank you for bringing out the Seventh Day Adventist (SDA) connection to the “plant-based” agenda that Katz et all espouse.
I first found out about the SDA church vegetarian agenda from reading Rhys Southan’s meticulously researched papers on his Let Them Eat Blog back in 2012.
http://letthemeatmeat.com/tagged/Seventhday_Adventists
I’m extremely glad the Fettke’s have taken up the torch and are extending this knowledge base.
We need REAL nutrition science, not the diet ramblings of a woman who mistook her brain dysfunction following a major head injury and three-week-long coma for messages from God.
If SDA people want to believe that Ellen White’s post brain injury writings were from God’s mouth to Ellen’s ears, fine. But don’t foist her nutrition beliefs on the entire population of the world and pretend it’s about science. It’s not. It’s religion. Period.
Hi Ben
Amen to that!
Best wishes – Zoe ;-)
WOW! That develops Gary Fettke’s points made in his video and on Marika’s blog to a whole other level.
Obviously they are only interested in “improving” the health of already healthy people.
“If thine eye offend thee, pluck it out! And while we’re at it we’ll take that foot, and the kidneys” pretty much sums up current attitudes to diabetes, well obviously diabetics are SINNERS for eating all that meat, and eggs. Completely logical, and completely wrong, yet being touted by all the Embedded Vegans who inhabit pretty much every low carb/keto blog and Twitter account.
I’ve wondered for a while now who actually coordinates their activities. They used to point to Plant Positive videos, then in lock step they switched to pointing to Greger. When they get into difficulties they call for Joel Kahn. Obviously they have backup also from dieticians, and believers in low fat and statins, who in turn have backup from the drug companies, carbohydrate processors and margarine manufacturers.
Note also that the SDA support sugar. Well obviously sugar, Coke and cornflakes are low fat and vegan, and O6 seed oils are vegan too.
I’ve actually seen “normal” Christians claiming that low carb diets are a direct insult to God because they cut out bread which is a biblically essential part of the diet, and that “Paleo” is wrong because there is no evolution . . .
Wow, the link to Gary’s research is very interesting, though if I talk to friends at work or family they still think I am some kind of conspiracy theorist so I will resist mentioning corn flakes came about to stop us masturbating ha ha.
On a serious note, I have been waiting for this second part, and will hold my hand up to sometimes getting mixed up between six countries and the seven countries study.
This has come very timely for me as I have just been appointed by Sam as the local ambassador in my area for the PHC and I know I am going to get asked why we follow this advice, so thank you Zoe.
Hey well done! Many thanks for your funny and nice comment :-)
There is a history of ‘health’ foods, tonics and evangelism (doesn’t have to be religious).
Kellog and his cornflakes; part of healthy lifestyle to stop you playing with yourself, same with Grahams Crackers I think
Muesli; Dr Bircher in Switzerland part of his health food plan.
Coca Cola; a tonic to make you feel good, not surprising as it had cocaine in it
Procter and Gamble; Crisco was sold as a sophisticated way to cook despite the fact that it was made from hydrolysed cotton seed.
I really appreciate your detailed work on this. Your points are clear yet for me it still takes a good deal of concentration and thinking to really understand. No wonder people are so easily bamboozled – the studies you dissect seem scientific and reasonable on the surface: as you show, it is only on the surface and only by ignoring contrary evidence.
Like Uffe Ravnskov’s book, “The Cholesterol Myths,” the way you dissect these papers becomes a case history on how these people manipulate study design, data and presentation to find conclusions that suit their beliefs and obfuscate the truth. Scary stuff.
I find it infuriating that people and organizations like the AHA simply ignore what they find inconvenient. They perpetuate myths that keep people from being healthy.
Thanks for doing what you do. And thanks for making great articles like this available to all.
Hi Michael
Thank you for your lovely comment :-)
Best wishes – Zoe
Dr. Harcombe
Your Parts 1 and 2 discourse of the White Paper/SCS is fascinating. After reviewing your sources myself, I find that you are on solid footing. Minimally, the saturated fat to CVD is baseless. Most interestingly, correlations to processed food should open the medical field’s eyes.
There are some rather significant benefactors of the low fat hypothesis that are involved in processed food. Dare I mention that the sugar and cereal industry, and grain-based industries make trillions of dollars yearly? Add the trillions yearly made in health care from obesity, diabetes, CVD, and cancer as a secondary outcome. If Dr Harcombe’s correlation to processed foods is right (and I’m confident that that will ultimately be discovered to be true), then she has hit on an answer for the current health care crisis by providing a preventable solution: eat real food.
Hi David
Thank you!
You may enjoy the work that the Fettkes have been doing looking into big money and big cereal (and religion!)
http://foodmed.net/2017/08/07/medical-evangelism-adventist-diet-advice/
Best wishes – Zoe
“Gary and Belinda Fettke …” Hm!
In response to a tweet from him about the movie “What the Health”, I tweeted “I’m now smoking 15 cigarettes for breakfast instead of 3 eggs. It is more expensive and I don’t feel well! Is it OK to go back to eggs?”
Using the robust scientific principles that dietitian-organisations use, (cherry-picking what he liked: “I’m now smoking 15 cigarettes for breakfast instead of 3 eggs”; ignoring the side-effects: “It is more expensive and I don’t feel well”; and not responding to questions: “Is it OK to go back to eggs?”), Gary “LIKED” my tweet. Proving that he is pro-smoking and anti-eggs!
(Chuckle!)
I’m a BIT suspicious of claims that religious groups had a big influence, at least IF that is about plant-based eating linked specifically linked to their religion. I’ve read that one religious leader was so keen that his followers ate fish that he performed miracles to ensure that they got enough. (OK, not lots of saturated fat, but some).
(And I would be a bit suspicious about any claims that religious people are in favour of continuous consumption of carbohydrates, when nearly all religions encourage that “modern fad” called “fasting”! But I don’t think that was being claimed here).
I DO feel that there is a puritan ideology behind some of the claims: the universe can’t possibly be arranged so that we can actually ENJOY our food and drink! Enjoy meat? Enjoy alcohol? No way! However, I think this puritanism is shared by some non-religious people too.
Barry – you’re naughty! LOL!
I don’t know how deep the Seventh Day stuff goes – that’s what the Fettkes have been discovering. I do think the plant-based/lifestyle medicine/medical evangelism stuff they have unearthed is very interesting and I do think pant-based is akin to religion in itself. The puritan bit is deffo there – started with Mr Kellogs not wanting anyone having fun or sex or suchlike!
Best wishes – Zoe